Abstract
Background: Management of intoxicated undergraduate students is challenging for higher education institutions. Refusal of care can be problematic due to the intoxicated undergraduate students’ lack of decision-making capacity. This study’s objective was to compare existing and desired transport policies for intoxicated undergraduate students among collegiate EMS agencies. Methods: A thirteen-question online survey was sent via e-mail to the medical directors of the 232 undergraduate emergency medical services agencies listed in the database of the National Collegiate Emergency Medical Services Foundation (NCEMSF). The e-mail provided a link to complete the survey. Follow-up phone calls and e-mails were performed after the initial email to assist with survey completion. The study occurred from April 2013 to March 2014. All of the responses were anonymous, and participation in the survey was voluntary. Responses for questions were totaled and percentages were calculated. Written responses were also reviewed. Two-sided tests of significance (p < 0.05) were performed on preference for transport policy. Results: The survey was sent to 232 agencies with 99 responding and 67 had an active undergraduate emergency medical services agency. Twenty-four percent require transport to the nearest emergency department (ED) (Option A); 24% allow for refusal of care with medical command (Option B); 48% allow for refusal of care without medical command (Option C); and 4% stated that the patient must be transported to a location other than the nearest ED (Option D). Among the 20 agencies who desired a change in current transport polices to preferred ones, there was a significant increase observed in preference toward medical command input (p = 0.03). Twenty percent stated that laws prevented policy modification. The policies or wishes of higher education institutions made alterations challenging in 50% of agencies. Conclusion: Variation in policies suggest that higher education institutions may have specific needs due to their unique campus operations and/or differences in state and local laws. Thirty percent of responding collegiate EMS agencies desired to change their transport policies. Further research should determine the specific barriers to implementing the preferred transportation policy of the medical director as well as the advantages and disadvantages of the various transport policies.
Introduction
Alcohol consumption is a condition that can lead to serious health consequences and injuries, which often necessitate prehospital emergency medical care for undergraduate students.1,2 Current undergraduate drinking culture encourages these levels of intoxication. It is estimated that one out of every fifteen undergraduate students will come to the emergency department with an alcohol related problem.3 College freshmen are particularly likely to present to the emergency department with an alcohol related illness or injury.4 Oftentimes, it is collegiate emergency medical services (EMS) agencies, staffed mostly by current students, who are responding to their intoxicated peers.
Collegiate EMS agencies are a unique model of delivering prehospital care because they function only in a university campus setting.5 Higher education institutions are responsible for the actions of collegiate EMS and their crews as well as for providing adequate resources. Alcohol misuse places resource demands on colleges and universities, often requiring the provision of medical services to intoxicated students, such as ambulance use and advanced life support. One in six campus-based ambulance runs is associated with alcohol misus.6 For higher education institutions supporting collegiate EMS agencies who provide free medical care, this cost becomes even more pronounced.
The presence of collegiate EMS on college campuses may promote a culture conducive to increased reporting behavior of intoxicated students, which leads to a safer, more transparent campus.7 Alcohol amnesty policies gradually implemented at universities are designed to protect the health of students by assuring them that they will not be subject to serious disciplinary or legal actions for obtaining medical care in their intoxicated state. However, such policies on campuses may possibly lead to more EMS transports of intoxicated undergraduate students since students may be more willing to call for medical assistance knowing that they will receive amnesty by doing so. This possibly signals the need for a better transport policy to appropriately care for this patient population.
Managing intoxicated undergraduate students is a challenge for higher education institutions due to issues of legal liability. Higher education institutions have a responsibility to provide a safe environment for their students to learn, but also to live and mature. Transporting intoxicated students to the nearest emergency department would ensure the greatest level of safety and minimize liability, but require involvement from more resources.
Refusal of medical care can also become problematic due to the intoxicated patient’s possible lack of decision-making capacity. Determining the transport destination policies of collegiate EMS agencies may be difficult due to the unique responsibilities of the higher education institutions for their students as listed in Table 1. EMS protocols for facilitating refusal of medical care vary based on state, local, and agency-specific/medical command-specific guidelines. Generally, in order to refuse medical care in the prehospital environment, a patient must be an alert and fully oriented (person, place, time, and event) adult of 18 years of age or older. The patient must also display decision-making capacity in the refusal process – the ability to recognize that they may suffer severe injury or loss of life if they refuse EMS care and/or transport. Patients showing any signs of altered mental status due to the consumption of drugs or alcohol may not be considered competent in their intoxicated state, and thus may not have legal capacity to refuse care (even if they are a fully alert and oriented adult).8
Table 1: Questions for Transport Policy Considerations
The biggest obscurity in this process lies in how an EMS provider determines whether drugs or alcohol have impaired their patient’s ability to make informed medical decisions. A mini-mental exam could be used in the assessment of a potentially altered patient’s ability to refuse medical care. Failure of the exam identifies the patient as currently unable to make medical decisions, and only specific orders from on-line medical command would refute these findings. Fundamentally, the patient would need to demonstrate decision-making capacity, which would consist of being awake, alert, and oriented to person, place, time, and event in addition to being lucid and capable of making an informed decision by demonstrating understanding, appreciation of the situation, reasoning, and the ability to express choice.
Alcohol-related illness and/or injury places increased burden on collegiate EMS agencies, their respective higher education institutions, and neighboring emergency departments, but it is important to acknowledge this for the betterment of collegiate EMS transport and patient outcomes. The objective of this study was to compare the existing and desired transport policies for intoxicated undergraduate students among undergraduate emergency medical services agencies across the United States.
Materials and Methods
A thirteen-question online survey (Supplementary Figure 1) was sent via e-mail to the medical directors of the 232 undergraduate emergency medical services agencies listed in the database of the National Collegiate Emergency Medical Services Foundation (NCEMSF). The survey focused on undergraduate students who were at least 18 years of age, intoxicated with alcohol, and who were evaluated by the undergraduate EMS agency. Patients who ingested other illicit substances were not referenced.
If an e-mail address was not available on the NCEMSF website, the e-mail address on the agency’s website was used if available. The e-mail provided a link to complete the survey. Follow-up phone calls using publicly available phone numbers and e-mails to the original email addresses were performed after the initial email to assist with survey completion using a formal script depending on whether the call was answered (Supplementary Figure 2).
The study occurred from April 2013 to March 2014. All of the responses were anonymous, and participation in the survey was voluntary. Responses for questions were totaled and percentages were calculated. Free text responses were also reviewed for context. Two-sided tests of significance (p < 0.05) were performed on preference for transport policy. The University Hospitals Institutional Review Board (IRB) deemed this study exempt.
Results
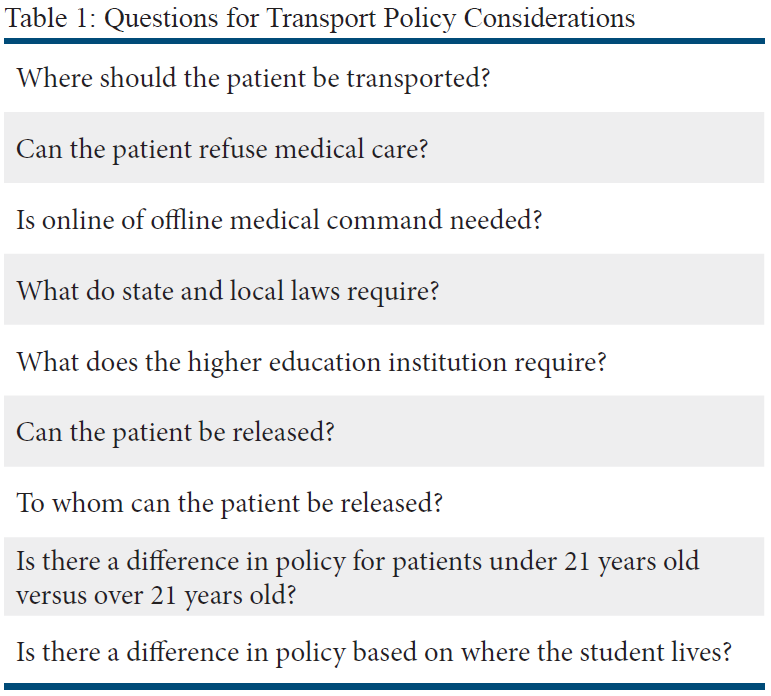
Of the 99 agencies that responded to the survey, 67 had an active undergraduate emergency medical services agency. Collegiate EMS policies regarding the transport of alcohol-intoxicated patients varied widely. As shown in Figure 1, sixteen agencies (24%) must transport the intoxicated student to the nearest ED (Option A). Another 16 agencies (24%) allow the patient to refuse medical assistance, but on-line medical command must be contacted and approve the refusal (Option B). Thirty-two agencies (48%) allow the patient to refuse medical assistance without on-line medical command approval (Option C). Three agencies (4%) stated that the patient must be transported, but to a location other than the nearest ED (Option D). State or local laws govern the policies of 21 of the responding agencies (31%) while the policies in 24 agencies (36%) are required by the higher education institution that operates the collegiate EMS agency.
Figure 1: Distribution of Current EMS Transport Policies
Among those respondents that chose Option D, one agency responded that if no medical emergency exists, the student is transported to its higher education institution’s 24/7 Primary Care Center staffed by two nurses. Another higher education institution had an on-campus inpatient unit staffed by nurses under online medical direction from a local hospital. Ambulatory intoxicated students are transported to this inpatient unit and those students who register above a blood alcohol level of 0.3 upon evaluation at the infirmary must be transported by ambulance to the local ED. A third agency responded that its higher education institution has a college health center, but patients must be able to ambulate to the health center on their own.
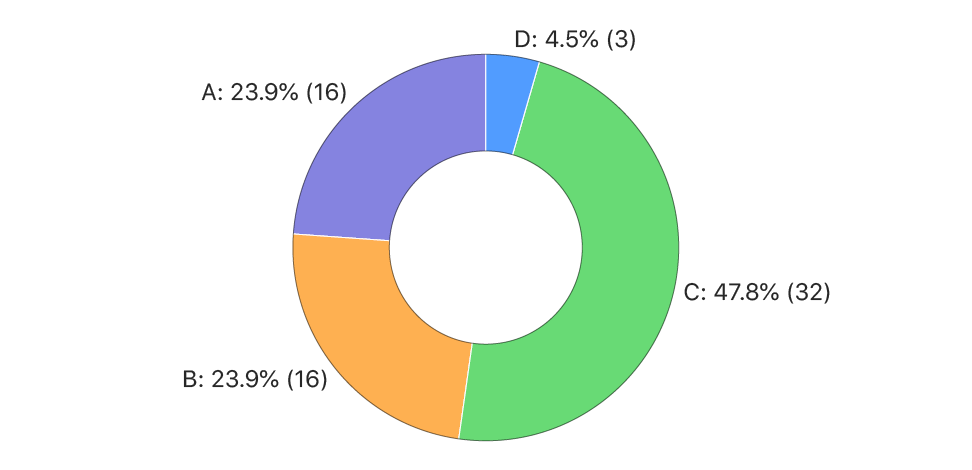
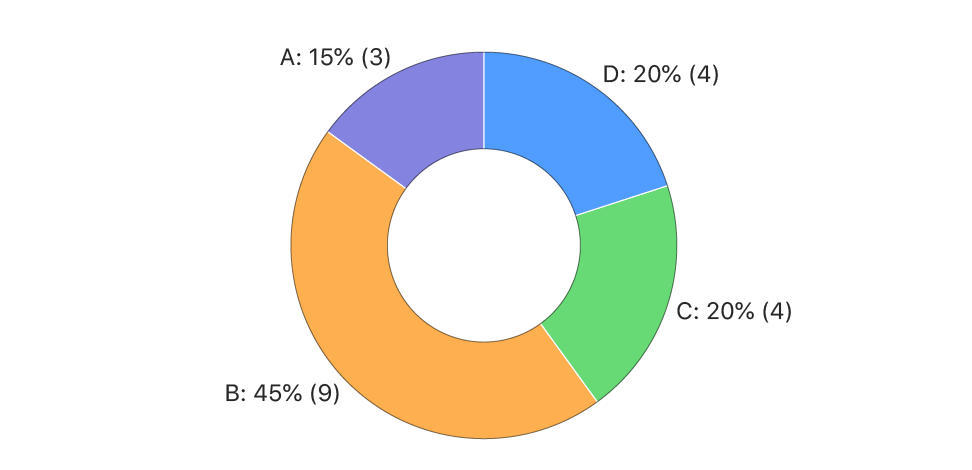
When asked about their preferred transportation policy, out of the 67 agencies who responded, 13 agencies (19%) chose Option A; 22 agencies (33%) chose Option B; 26 agencies (39%) chose Option C; and 6 agencies (9%) chose Option D (Figure 2). Among those agencies that chose Option D, two respondents preferred that the patients be taken to the campus health center to be supervised by a nurse unless other issues existed. Three other respondents preferred an on-campus detoxification center supervised by medical providers.
Figure 2: Distribution of Preferred EMS Transportation Policies
Twenty of the responding 67 agencies (30%) desired to change their current transport policies for intoxicated undergraduate students. Among these 20 agencies, 6 (30%) selected Option A; 3 (15%) chose Option B; 10 (50%) allowed for Option C; and one (5%) selected Option D (Figure 3). When asked about their preferred transportation policy, 3 (15%) selected Option A; 9 (45%) chose Option B; 4 (20%) allowed for Option C; and 4 (20%) selected Option D (Figure 4). Comparing current transport policy to desired transport policy, there was a significant increase observed toward medical command input for refusal of care (p = 0.03).
Figure 3: Distribution of Current Transport Policies for Agencies who Desire to Change Transport Policies to Preferred Transport Policies
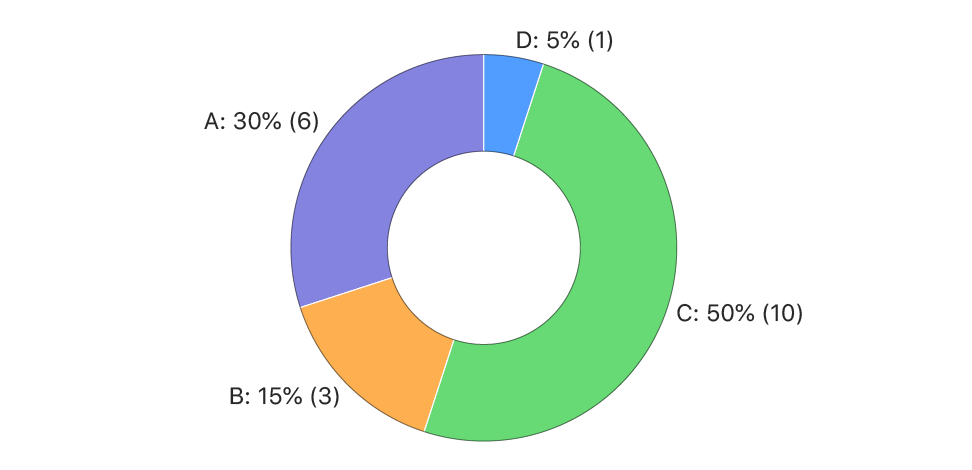
Figure 4: Distribution of Preferred Transport Policies for Agencies who Desire to Change Transport Policies to Preferred Trasport Policies
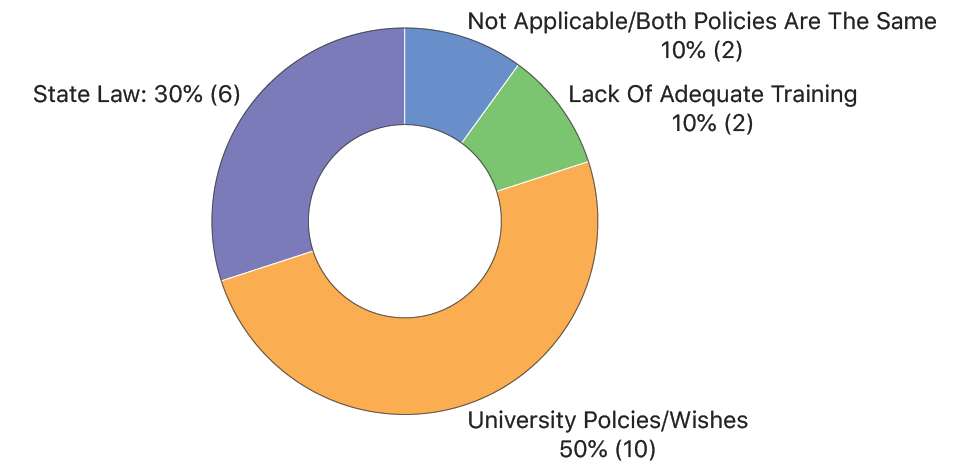
As shown in Figure 5, of the same 20 agencies, 6 (20%) stated that state/local laws prevented reform of their current transportation policy, while the policies or wishes of higher HEIs were obstacles in 10 (50%) of agencies. Only 2 agencies (10%) felt that lack of adequate training for their EMS crew was a primary challenge to transportation policy reform. Two agencies (10%) indicated that both polices were the same even though their choices to the previous relevant questions showed a difference between their current and preferred EMS transport policies.
Figure 5: Distribution of Obstacles/Challenges for Implementing Preferred Transport Policy
In 32 of the 67 responding agencies (48%), an undergraduate student over 18 years old can be released into the custody of a friend and/or roommate for observation. In only 26 agencies (39%) can the undergraduate student over 18 years old be released into the custody of a dorm resident advisor/counselor.
Fifty-nine agencies (88%) did not have differing policies for students who are under 21 years old versus students who are over 21 years old. Among those agencies that did have differing policies, one agency stated that an intoxicated student over 21 years old can be released to a sober friend over 21 years old as long as no life-threatening emergency exists. One agency stated that its higher education institution has a medical amnesty policy for all students, but those under 21 years of age have to meet with the dean. At a different higher education institution, students under the age of 21 years old may face disciplinary actions and possible legal charges per the university student agreement with police. Another agency responded that intoxicated students between 18 and 21 years of age require transport to the nearest healthcare facility, unless they are determined not to be acutely intoxicated following a medical assessment, while those patients over 21 years of age would be turned over to the police department if found to be acutely intoxicated and refused transport to the nearest healthcare facility; police would place them in protective custody if warranted. At one higher education institution, students older than 21 years old can sign a refusal if they meet certain criteria, but medical control must be contacted and approve the refusal.
Six of the responding agencies (9%) had differing policies based on where the student lives, such as a dorm, fraternity or sorority housing, or off-campus housing. One agency stated that those who live off-campus are not subject to the higher education institution’s policy in which the patient cannot be left with a friend to monitor sobriety. Another agency responded that since fraternity and sorority housing is located outside of university property, students who live in these houses are subject to the city code rules and regulations on intoxication. At another higher education institution, off-campus housing is not under the jurisdiction of campus police, so the city fire/ambulance service responds. The local police at one higher education institution requests that campus security, who are non-sworn officers, must call the local police for any off campus housing emergency, including calls related to intoxication. The police on scene will then request that the town fire department transport the patient to the emergency department or allow the campus EMS agency to bring the student to the on-campus infirmary after the student has been issued a citation and/or summons.
Discussion
Approximately 30% of responding undergraduate EMS agencies have a current alcohol transport policy their respective medical directors would like to amend. Of the 20 agencies desiring a change in policy, most prefer a policy that allows for refusal of care. Of the agencies that want to include refusal as an option, a majority want this refusal process to be completed under the oversight of an on-line medical command physician. When transport becomes pertinent, no preference was shown between transport to the nearest ED or to an alternate location (detoxification center, other ED, etc.). Barriers towards eliciting these desired protocol changes reportedly lie within the current policies/wishes of respective higher education institutions and somewhat within the current state and local laws.
Many intoxicated patients are taken to the emergency department. One study examined demographic and clinical features of alcohol-related visits for patients who were enrolled as undergraduates at a 4-year public higher education institution during 2 academic years.1 Enrollment was approximately 12,500 undergraduates per year. The authors found that of all undergraduate emergency department visits, 13% were alcohol- related. Of all undergraduate students who presented to the ED, 0.7% presented with alcohol-related medical conditions each year. Injuries accounted for 53% of all visits. Acute intoxication accounted for 34% of all visits. Only nine of 185 patients were hospitalized. Men 21 years and older had the highest odds of visiting the ED, and trauma occurred more frequently among men, students > 18 years old, and white students with 84% due to accidents an 16% due to fights. Acute intoxication occurred more frequently among women, students < 18 years old, and nonwhite students.
Many students transported to the ED do not always need emergent care. A 2017 study investigated the extent to which intoxicated patients transported by South Korean EMS received ED treatment once at the hospital.9 Separated into non-intoxicated (n=120) and intoxicated (n=92) groups, 70.7% of the intoxicated patients did not receive ED treatment against medical advice: 10.9% refused, 52.2% were uncooperative, and 7.6% wanted a transfer to another hospital. Of the 29.3% of intoxicated patients who did not receive care based on physician recommendation, 5.4% were simply in a drunken state, 10.9% could be treated in an outpatient department, and 13% showed the same symptoms on repeated visits.
A study conducted in 2005-2006 reviewed medical records of University Health Service (UHS) admissions with McLean Hospital and Harvard University.10 One hundred students were admitted in the after-hours acute care service for alcohol intoxication, with 78% of students below the legal drinking age and 48% of students being freshmen. Five students were sent to the ED for further care, and 30 students were sent directly to the ED without even being seen first at UHS due to higher intoxication levels or increased combativeness. 65% of students did not go to the ED. 10% of students were admitted to urgent care more than once during the study period of approximately 6 months. Complete medical records of some of these students were utilized, with 31.3% reporting anxiety in the 2 weeks prior to admission. This study is encouraging in the development of a 24-hour acute care service on campuses that can treat and manage a majority of students admitted for alcohol intoxication. The use of this university service would release EDs from some of the localized burden of undergraduate drinkers, while still allowing for students to detox in a medically supervised, university-approved manner, thus relieving liability concerns. This proposed solution requires further thought into how exactly an EMS provider can determine the appropriate destination for their intoxicated student with a proper level of care.
A study conducted between the academic years of 2007 and 2011 evaluated undergraduate students transported to local EDs with data compiled by Boston Medical Center.11 92% of students (ntotal=971) had their alcohol content measured either by breath or blood. Almost all students were over the legal limit to drive a car in the United States (if they were of age) and a fifth of students were at least 3.1 times the legal limit. For EMS personnel, the use of blood alcohol concentration (BAC) readings is often not the first priority, as each individual will process similar amounts of alcohol differently and present with varying levels of impairment. Despite the possible inconsistency with BAC and a patient’s competency level, the addition of blood alcohol content measurements to evaluate intoxication in college undergraduates warrants further study.
Few studies address a possible lack of education or need for further training of all EMS agencies (not just collegiate EMS agencies) on refusal proceedings for the intoxicated patient. This is not stated in a negative way or as to put EMS providers’ decisions in question. It is possible that a more specific set of guidelines for refusal of the intoxicated patient needs to be developed, and that the current methods, as outlined previously, are too ambiguous for a consistent standard of care to be maintained.
A study conducted on EMS agencies of El Paso County, Colorado tested the use of a “detoxification evaluation checklist” as a tool for determining intoxicated patients (with no other prominent presentation) as candidates for transport to a local detoxification center, as opposed to a hospital emergency department.12 This checklist consists of 29 yes or no questions focusing on patient cooperation level, recognition of significant medical history, and outlining vital sign limitations. Requiring a crew signature, receiving signature, and report number, this checklist clearly a clinical tool for clearing patients from ED specific care (a “yes” answer to any question disqualifies the patient from detoxification center transport). 19% of patients were able to go to the detoxification center, with only 3% of these patients having adverse effects that required subsequent ED transport. This study suggests that with specific guidelines, EMS is able to determine a patient’s candidacy for alternative detox care. In the case of collegiate EMS agencies operating under higher education institutions, detoxification centers may not be present or included as an appropriate destination in higher education institution policy. Additionally, emergency departments are typically the only 24-hour care facilities available on or near campuses.
Medical amnesty programs at higher education institutions have also been controversial due to the tension between the responsibility of the higher education institution to enforce the minimum legal drinking age of 21 years ago as well as other applicable laws and policies vs. the need to remove barriers so that students will call for assistance in alcohol-related emergencies. One paper examining a single university’s Medical Amnesty Protocol (MAP) showed an increase in the percentage of students who reported calling for help on behalf of an intoxicated person from 4.5% before the protocol to 6.8% during the first year of the protocol and 5.4% during the second year.13 Furthermore, the MAP led to a decrease in students who reported that they did not call for help in an alcohol-related emergency because they “didn’t want to get the person in trouble” from 3.8% before the protocol to 1.5% after two years of protocol implementation.13 The authors also reported that the number of alcohol-related calls to the higher education institution’s EMS increased each year after the implementation of the MAP, likely due to the MAP motivating students to call for help by reducing fear of judicial consequences rather than an increased number of severe intoxication cases.
Another study evaluated call volumes for a collegiate EMS agency before and after a MAP was initiated. They found a higher call volume per day (0.84 vs. 0.93 p < 0.01); requests for service that occurred earlier in the evening; and a reduction in ALS requests for alcohol-related emergencies (9.0% vs. 3.7%: OR 0.39; p < 0.01).14 Nevertheless, higher education institutions need to place greater attention on how MAPs are implemented, communicated, and interpreted. One study examined students’ awareness of its MAP and the influence of this awareness on the expected consequences of bystander help seeking in alcohol-related emergencies among student-athletes and non-athletes.15 Among 1,012 college students, 25% were unsure if their school had a MAP. Of these students, 67% attended schools with a MAP. These students who were unsure of an MAP were more likely to expect serious negative consequences of calling for help for both non-athlete peers (Beta = 1.152, p < 0.001) and student-athlete peers (Beta = 0.887, p = 0.001).
Limitations
addition, this study was conducted several years ago. Accordingly, collegiate EMS transport policies for intoxicated undergraduate students may have changed since this study was conducted. Another limitation is that only 67 of the 99 responding agencies have transport capabilities. It is possible that these non-transport agencies could have treatment and refusal of care policies for intoxicated students.
Other limitations include difficulties in capturing heterogeneity in policies and a lack of follow-up questions to better understand preferred transport policies. Such questions might have included what specific changes medical directors would like to make to current transport policies.
Conclusion
It is advisable for medical directors to communicate with HEI administrators to develop policies that are agreeable to both parties and have the patient’s best interest in mind. Variation in policies suggest that higher education institutions may have specific needs due to their unique campus operations and/or differences in state and local laws. Nevertheless, consensus on national guidelines should be explored for the possible standardization of the transport of intoxicated undergraduate students. Further research should determine the specific barriers to implementing the preferred transportation policy of the medical director as well as the advantages and disadvantages of the various transport policies. The role of the collegiate EMS agency in forming transport policy guidelines should also be investigated through discussions at the national level and through national organizations regarding the best practices for the transport of intoxicated undergraduate students by collegiate EMS agencies.
References
- Turner JC, Shu J: Serious health consequences associated with alcohol use among college students: demographic and clinical characteristics of patients seen in an emergency department. J Stud Alcohol 2004, 65(2):179-183.
- McLaughlin MP: Alcohol-associated illness and injury and ambulance calls in a midwestern college town: a four-year retrospective analysis. Prehosp Emerg Care 2010, 14(4):485-490.
- Wright SW, Norton VC, Dake AD, Pinkston JR, Slovis CM: Alcohol on campus: alcohol-related emergencies in undergraduate college students. South Med J 1998, 91(10):909-913.
- Wright SW, Slovis CM: Drinking on campus. Undergraduate intoxication requiring emergency care. Arch Pediatr Adolesc Med 1996, 150(7):699-702.
- Fisher J, Ray A, Savett SC, Milliron ME, Koenig GJ: Collegiate-based emergency medical services (EMS): a survey of EMS systems on college campuses. Prehosp Disaster Med 2006, 21(2):91-96.
- Carey KB, McClurg AJ, Bolles JR, Hubbell SJ, Will HA, Carey MP: College student drinking and ambulance utilization. J Public Health Manag Pract 2009, 15(6):524-528.
- Rosen JB, Olson MH, Kelly M: Collegiate-based emergency medical service: impact on alcohol-related emergency department transports at a small liberal arts college. J Am Coll Health 2012, 60(3):263-265.
- Mistovich JJ, Karren KJ: Prehospital Emergency Care, 11 edn. Boston: Brady/Pearson; 2018.
- Van Dillen C, Kim SH: Unnecessary emergency medical services transport associated with alcohol intoxication. J Int Med Res 2018, 46(1):33-43.
- Benningfield MM, Trucco EM, Barreira PJ, Greenfield SF: Treatment of Alcohol Intoxication at University Health Services: Examining Clinical Characteristics, Drinking Patterns, and Adherence with Referral. J Alcohol Drug Educ 2009, 53(1):54-69.
- Kharasch SJ, McBride DR, Saitz R, Myers WP: Drinking to toxicity: college students referred for emergency medical evaluation. Addict Sci Clin Pract 2016, 11(1):11.
- Ross DW, Schullek JR, Homan MB: EMS triage and transport of intoxicated individuals to a detoxification facility instead of an emergency department. Ann Emerg Med 2013, 61(2):175-184.
- Lewis DK, Marchell TC: Safety first: A medical amnesty approach to alcohol poisoning at a U.S. university. International Journal of Drug Policy 2006, 17(4):329-338.
- Monahan BV, Nable JV, WinklerPrins V: Implementation of an Alcohol Medical Amnesty Policy at an Urban University With a Collegiate-Based Emergency Medical Services Agency. J Adolesc Health 2019, 64(1):134-136.
- Weaver GM, Kroshus E, Milroy J, Wyrick D: Student awareness of campus medical amnesty policies. J Am Coll Health 2020:1-8.
Supplementary Materials
Supplementary Figure 1: Online Survey
Supplementary Figure 2: Phone Call Script
Author & Article Information
Jamie Shah, BA graduated with a BA in Anthropology from Case Western Reserve University and is currently a fourth-year medical student at Kansas City University of Medicine and Biosciences. William Qu, MD graduated in May 2020 from Emory University School of Medicine and is currently a first-year resident at Emory’s Integrated Cardiothoracic Surgery Residency Program. Anise Bowman, BA, graduated with a BA in Biochemistry and Environment Studies from Case Western Reserve University and is currently a second-year medical student at CWRU School of Medicine. Eleanor Wilson, BA graduated with a BA in biology from Case Western Reserve University and is currently a second-year medical student at the University of Pikeville Kentucky College of Osteopathic Medicine. Jeffrey Luk, MD, MS, FACEP, FAEMS is the Director of Prehospital and Disaster Medicine in the Department of Emergency Medicine at University Hospitals Cleveland Medical Center. He is an Associate Professor of Emergency Medicine at the Case Western Reserve University School of Medicine. He has served as Medical Director for CWRU EMS since August 2011
Author Affiliations: From Case Western Reserve University – in Cleveland, OH (J.S., W.Q. A.B. E.W.). From Case Western University; Department of Emergency Medicine, University Hospitals Cleveland Medical Center – in Cleveland OH (J.L.).
Address for Correspondence: Jeffrey Luk | Email: jhlukmd@gmail.com
Conflicts of Interest/Funding Sources: By the JCEMS Submission Declaration Form, all authors are required to disclose all potential conflicts of interest and funding sources. All authors disclosed their affiliation with the University of Arizona Emergency Medical Services and declared no other conflicts of interest. All authors declared that they did not receive funding to conduct this research and/or associated with this work.
Authorship Criteria: By the JCEMS Submission Declaration Form, all authors are required to attest to meeting the four ICMJE.org authorship criteria: (1) Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND (2) Drafting the work or revising it critically for important intellectual content; AND (3) Final approval of the version to be published; AND (4) Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Submission History: Received August 2, 2020; accepted for publication January 26, 2022
Published Online: November 30, 2022
Published in Print: November 30, 2022 (Volume 5: Issue 2)
Reviewer Information: In accordance with JCEMS editorial policy, Original Research manuscripts undergo double-blind peer-review by at least two independent reviewers. JCEMS thanks the anonymous reviewers who contributed to the review of this work.
Copyright: © 2022 Shah, Qu, Bowman, Wilson, & Luk. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International (CC BY 4.0) License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. The full license is available at: https://creativecommons.org/licenses/by/4.0/
Electronic Link: https://doi.org/10.30542/JCEMS.2022.05.02.03