Abstract
Introduction: While the impact that the social determinants of health have on a patient’s healthcare experience have been repeatedly proven1, there is little existing literature describing how these determinants impact a patient’s willingness to engage with and their perception of the healthcare system, particularly with regards to emergent transport to an emergency department. Study Objective: The goal of this experiment is to determine if age and gender exert significant influence on a patient’s decision to utilize ambulatory transport to the emergency department. Methods: Data from PCRs generated by the University of Arizona Emergency Medical Services from September 2018 to April 2021 was collected and used to sort each PCR by patient age, gender and final transport decision. Statistical analysis (through a χ2 test of independence and logistic regression) was performed to determine if statistically significant variations in transportation rates exist as a result of age and gender differences. Results: The χ2 test of independence for gender demonstrated a high likelihood that the variation observed was due to chance (p = 0.140), while the logistic regression test regarding age and transportation decision revealed a strong correlation between age and ambulance usage (p = 0.0007). Conclusion: For the calls analyzed herein, age potentially has a strong linear association with a patient’s decision to utilize an ambulance for transportation to the emergency department, with the likelihood of transport increasing as a patient’s age increased. Gender was found to have no significant relationship in transport outcome.
Introduction
Social determinants of health refer to the specific conditions of a patient’s life (education, living environment, financial status, etc.) that directly and indirectly affect a patient’s healthcare experience.2 The effects that social determinants of health inflict upon a person contribute to health inequalities. Only recently have studies focused on the role these factors play.1,3 Recent research has shown connections between a patient’s determinants and their healthcare-related outcomes; this is the case for clearly-defined metrics (life expectancy) and more intangible measurements (such as a patient’s overall stress).1 These factors have also been associated with varying perspectives on a patient’s healthcare interactions,4 potentially resulting from poor-quality care received in the past.5 This resulting hesitancy to engage with healthcare resources can compound healthcare inequalities.6 While some research has been performed regarding the effect age has on a patient’s decision to utilize emergent transport after motor-vehicle accidents,7 and the decision to pursue alternative destinations to the Emergency Department for medical care,8 the impact of age and gender remains poorly-researched.
The goal of this experiment is to explore further the relationship a patient’s social determinants have on their medical decision-making process; specifically, the purpose of this study is to examine the impact that age and gender have on a patient’s decision to utilize emergent transportation to an emergency department at the conclusion of a 9-1-1 call made from a university campus. While this decision represents a small part of a patient’s overall interaction with the healthcare system, it provides a simplistic binary result, facilitating comparisons across patient demographic groups.
Materials and Methods
A total of 2,283 Patient Care Reports were generated by the University of Arizona Emergency Medical Services (UAEMS) between September 2018 and April 2021; UAEMS is the University of Arizona’s collegiate EMS agency that responds to medical 9-1-1 calls originating on and directly adjacent to the college campus.9 Data from these call records was extracted using the Report Writer functionality of ImageTrend, an interface that allows for generating reports containing the minimal information requested.10 The data collected did not include identifiable markers, and as a result, exposure to Personal Health Information was avoided using this method.
Further criteria were imposed to ensure each PCR involved an incident in which the patient was determined to be competent and able to make an informed healthcare decision. In any situation where the patient does not possess the capacity to make an informed healthcare decision, transport determination is usually deferred to the healthcare providers on the scene.11 When notated, all calls with an assessment other than Alert on the Alert, Verbal, Painful, Unconscious Scale (AVPU Scale) were excluded from this study as a result. Additionally, PCRs involving patients with an inhibited level of consciousness were also excluded from this study. Assessment of this is performed on-scene by medical providers through four questions designed to discern alertness and orientation to the patient’s name, current location, current time, and current event; any patient assessed as “confused” or otherwise altered from normal mental baseline was considered to have an inhibited level of consciousness, causing exclusion. Finally, any calls in which the final transport decision was not notated were excluded from this study.
Of the 2,283 PCRs generated by UAEMS between September 2018 and April 2021, 1,153 calls fit the above inclusion criteria. Each patient’s gender and age were collected from each PCR and collated into categories separated by transport decision. This data was then evaluated using a χ2 test of independence12 and logistical regression analysis to determine if there was a linear pattern.
Results
Table 1 contains the distribution of patients with regards to gender. The values in parentheses represent the “expected” distribution of patients for each respective category. The resulting p-value from the χ2 test of independence is 0.140.
Table 1: All 1,153 patients sorted by gender and final transport decision, with “non-transport” referring to any decision not involving emergent transportation via ambulance to an emergency department
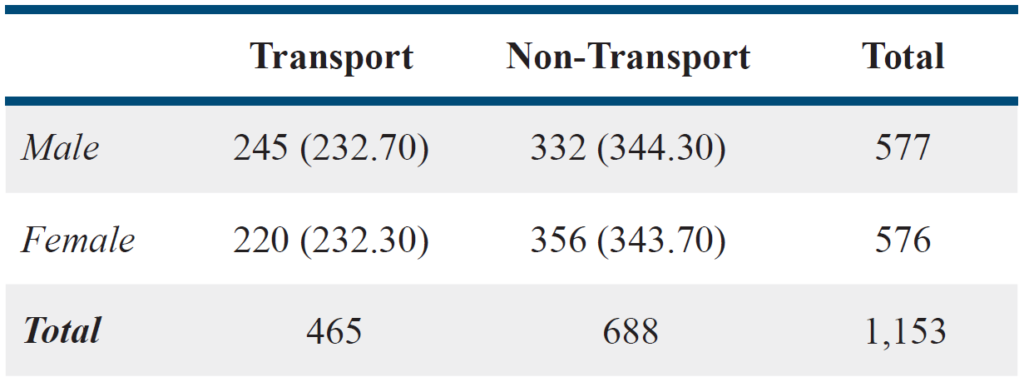
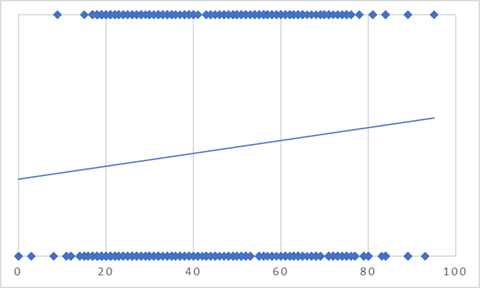
Figure 1 illustrates age compared to transportation outcome. Per the analysis, the calculated percentage of emergent transports to the hospital increases from 32.35% to 57.42% from birth to age 95 (the oldest patient included in this study). The p-value of the regression is 0.0007, representing an extremely strong association.
Figure 1: The graphed logistic regression of transport outcome as a binary function of age (emergent transport corresponding to a value of 1, all other outcomes to a value of 0)
Discussion
While the cut-off for a “statistically significant” p-value is variable, 0.05 has been found to be a reasonable set point for determining statistical significance.13 With a p-value of 0.14, we are unable to conclude that the variation in ambulance usage rates between gender isn’t due to random chance. Due to the high p-value from the test of independence regarding gender, we are unable to reject the null hypothesis that gender has no significant impact on a patient’s decision to utilize emergent transportation. The significantly lower p-value from the logistic regression in Figure 1 (0.0007) allows us to conclude that age has a statistically significant impact on a patient’s decision to utilize emergent transportation, specifically a linear relationship increasing the likelihood of emergent transport as patient age increases. Increased prehospital resource usage with older populations has been shown to be a result of increased medical problems rather than traumatic calls;14 however, further research must still be performed to see if this is applicable for the increased transport rate of older patients.
Limitations
While UAEMS responds to emergency medical calls outside the University of Arizona campus, the majority of patients seen by UAEMS are related to the University of Arizona and are likely college students. As a result, it is possible that the results found in this study may be affected by unique confounding factors present on higher education campuses or even factors specific to the Tucson, Arizona area. Additionally, the collegiate nature of UAEMS’s response zone limits the number of pediatric and geriatric patients seen, resulting in smaller sample sizes. Patient decisions beyond emergent transport outcomes were not recorded, and as such the utilization of alternative destinations is unable to be investigated.
Finally, while the mental status of a patient was a controlled variable for this experiment, the severity of the injury causing a 911-response was not; it is possible that older patients may present with more emergent injuries/medical conditions, skewing the percentage of patients who chose emergent transportation.
Conclusion
For the patient population present at the University of Arizona campus, age potentially has a statistically significant, and linear, impact on a patient’s decision to utilize emergent transport to the Emergency Department; gender has no statistically significant impact on this decision.
Acknowledgements
The authors would like to thank Emily Goldberg for their contributions to this research study. The authors would also like to acknowledge the University of Arizona Emergency Medical Services for their continued dedication to the safety and well-being of the University of Arizona campus.
References
- Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annual Review of Public Health. 2011;32(1):381-398. doi:10.1146/annurev-publhealth-031210-101218
- Social Determinants of Health. Social determinants of health – healthy people 2030. https://health.gov/healthypeople/objectives-and-data/social-determinants-health. Accessed February 20, 2022.
- Manuel, J. I. Racial/ethnic and gender disparities in health care use and access. Health Services Research. 2017;53(3):1407–1429. https://doi.org/10.1111/1475-6773.12705
- DeVoe JE, Wallace LS, Fryer GE Jr. Patient age influences perceptions about health care communication. Fam Med. 2009;41(2):126-133.
- Street RL, Elwyn G, Epstein RM. Patient preferences and healthcare outcomes: an ecological perspective. Expert Review of Pharmacoeconomics & Outcomes Research. 2012;12(2):167-180. doi:10.1586/erp.12.3
- Murray TM. Trust in African Americans’ healthcare experiences. Nurs Forum. 2015;50(4):285-292. doi:10.1111/nuf.12120
- Hunold KM, Sochor MR, McLean SA, Mosteller KB, Fernandez AR, Platts-Mills TF. Ambulance transport rates after motor vehicle collision for older vs. younger adults: a population-based study. Accident Analysis & Prevention. 2014;73:373-379. doi:10.1016/j.aap.2014.09.026
- Jones, C. M., Wasserman, E. B., Li, T., & Shah, M. N. Acceptability of alternatives to traditional emergency care: patient characteristics, alternate transport modes, and alternate destinations. Prehospital Emergency Care. 2015;19(4):516–523. https://doi.org/10.3109/10903127.2015.1025156
- Bradshaw H, Wright B, Carrasco B, Wise J, Gustafson T, Robishaw-Denton J. Comparing Patient Evaluations by a Municipal and a Collegiate-Based Emergency Medical Service. J Coll Emerg Med Serv. 2022;5(1). doi:10.30542/JCEMS.2022.05.01.04
- ImageTrend Report Writer – Creating a Report. August 2010.
- StatPearls. (2021, May 16). EMS Legal and Ethical Issues. StatPearls. https://www.statpearls.com/ArticleLibrary/viewarticle/31761
- McHugh ML. The chi-square test of Independence. Biochemia Medica. 2013;143-149. doi:10.11613/bm.2013.018
- Andrade C. The P value and statistical significance: misunderstandings, explanations, challenges, and alternatives. Indian J Psychol Med. 2019;41(3):210-215. doi:10.4103/IJPSYM.IJPSYM_193_19
- McConnel CE, Wilson RW. The demand for prehospital emergency services in an aging society. Soc Sci Med. 1998;46(8):1027-1031. doi:10.1016/s0277-9536(97)10029-6
Author & Article Information
Hans Bradshaw, MD is an Assistant Professor of Emergency Medicine and Pediatrics and serves as the Emergency Medicine Clerkship Director at the University of Arizona College of Medicine-Tucson. Dr. Bradshaw currently also serves as the Medical Director for the University of Arizona Emergency Medical Services. Jacob Robishaw-Denton, BS, EMT-B is a second-year medical student at the University of Arizona College of Medicine-Tucson and previously held the position of Deputy Chief of Operations at the University of Arizona Emergency Medical Services. Bianca Carrasco, BS, BA, EMT-B, is a current graduate student and the current Chief and Executive Director at the University of Arizona Emergency Medical Services. Timothy Gustafson, MPH, EMT-B, is a post-graduate from the University of Arizona and previously held the position of Chief and Executive Director at the University of Arizona Emergency Medical Services.
Author Affiliations: From University of Arizona College of Medicine; University of Arizona Emergency Medical Services – in Tucson, AZ (H.B., J.R.). From University of Arizona Emergency Medical Services; University of Arizona – in Tucson, AZ (B.C., T.G.).
Address for Correspondence: Jacob Robishaw-Denton | Email: jkdenton16@email.arizona.edu | Mailing Address: University of Arizona Emergency Medical Services, 1715 E 7th Street, Tucson, AZ 85719, USA
Conflicts of Interest/Funding Sources: By the JCEMS Submission Declaration Form, all authors are required to disclose all potential conflicts of interest and funding sources. All authors disclosed their affiliation with the University of Arizona Emergency Medical Services and declared no other conflicts of interest. All authors declared that they did not receive funding to conduct this research and/or associated with this work.
Authorship Criteria: By the JCEMS Submission Declaration Form, all authors are required to attest to meeting the four ICMJE.org authorship criteria: (1) Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND (2) Drafting the work or revising it critically for important intellectual content; AND (3) Final approval of the version to be published; AND (4) Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Submission History: Received May 17, 2022; accepted for publication June 15, 2022
Published Online: November 30, 2022
Published in Print: November 30, 2022 (Volume 5: Issue 2)
Reviewer Information: In accordance with JCEMS editorial policy, Original Research manuscripts undergo double-blind peer-review by at least two independent reviewers. JCEMS thanks the anonymous reviewers who contributed to the review of this work.
Copyright: © 2022 Bradshaw, Robishaw-Denton, Carrasco, & Gustafson. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International (CC BY 4.0) License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. The full license is available at: https://creativecommons.org/licenses/by/4.0/
Electronic Link: https://doi.org/10.30542/JCEMS.2022.05.02.02