| Download PDF (Available Soon) | |
| Author and Article Information |
Introduction
The life of a collegiate EMS provider is unique. Navigating post-secondary education while working long shifts in the prehospital world of complex medical emergencies is undeniably challenging. Treating patients experiencing physical trauma, mental health crises, or sudden medical emergencies requires superb training. More importantly, it demands true resilience to work these often-unpaid positions.
Following conversations with student leaders of collegiate EMS teams at a roundtable discussion at the 2023 National Collegiate Emergency Medical Services Foundation conference, it is clear that the stressful life of a collegiate EMS provider leads to service-level complications. Collegiate EMS leaders reported poor retention levels, which heightens the workload for the remaining service members, thus contributing to burnout. This destructive positive feedback loop also negatively affects patient safety (Hall, 2016).
Collegiate EMS team leaders have employed strategies in attempt to promote retention. Strategies mentioned at the roundtable discussion included balancing hours, demonstrating appreciation, and offering professional development opportunities. However, we believe the most crucial means of promoting retention is hiring providers who are well-prepared for the life of a collegiate EMS provider—those who are highly resilient and capable of growth. McMaster University’s Emergency First Response Team (EFRT) has curated a multi-step, highly selective hiring process in which we boast exemplary retention rates.
This article outlines our hiring process at McMaster University’s Emergency First Response Team (EFRT). Other collegiate EMS teams may replicate or adapt it to reduce retention complications and promote the quality of care provided to their community.
Hiring Process Overview
Our hiring process includes four phases, each described below. See Figure 1 for a hiring flowchart.
Figure 1: Hiring process flowchart
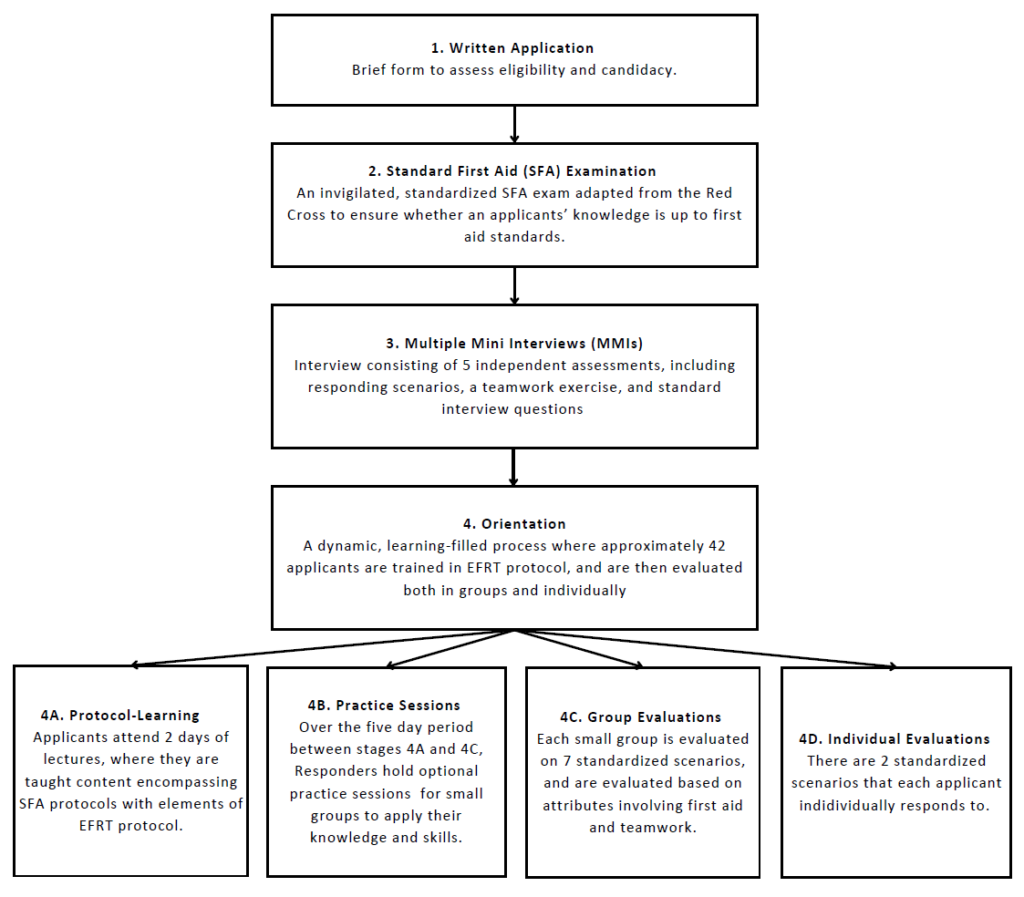
Phase 1: Written Application
The application process begins with an online written application involving
demographic (e.g., program, academic year), eligibility (e.g., full-time student status, certification requirements), and short answer questions (e.g., scenarios that assess teamwork, communication, and time management). We require applicants to hold a valid Standard First Aid (SFA) with CPR-C certification. There is no prerequisite experience necessary. Approximately 90% of applicants advance to Phase 2, as applicants are only screened out for ineligibility or evidence of inadequate soft skills (e.g., teamwork, communication, time management).
Phase 2: SFA Written Test
All applicants individually complete an identical 60-minute SFA Written Test consisting of 20 multiple-choice questions and two situational short-answer questions. Multiple choice questions are obtained from the Canadian Red Cross’ question bank for SFA Tests, while short answer questions are created by the EFRT. The Canadian Red Cross question bank can only be accessed by individuals with valid SFA Instructor certification through the Canadian Red Cross. The question bank is found online through Boulevard, a feature on the Canadian Red Cross website. The rubric for the short answer questions is created from the Canadian Red Cross SFA learning standards (The Canadian Red Cross Society, 2024). The top-scoring 80 applicants are invited to the next phase.
Phase 3: Multiple Mini Interviews (MMIs)
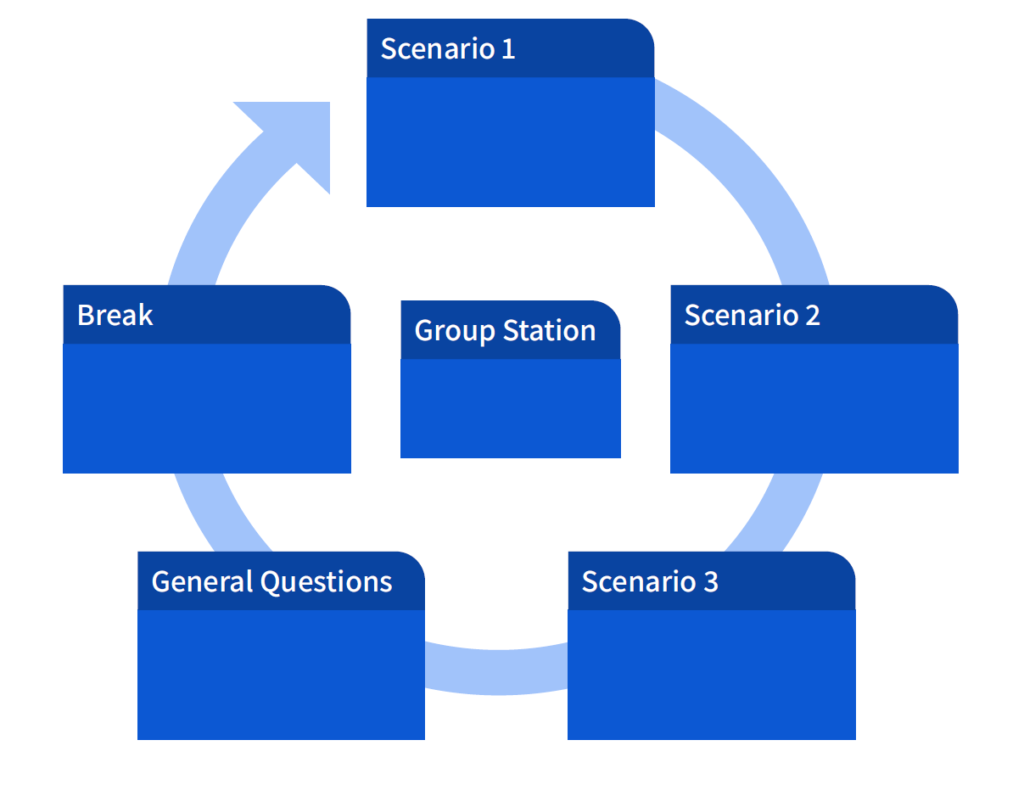
In MMIs, applicants undergo five interview stations. In each station, applicants are scored based on a standardized rubric that includes explicit actions/time limits that would yield a specific score. There are three simulated scenarios involving standardized patients to holistically assess the application of first aid skills alongside soft skills (e.g., active listening, responding empathetically, demeanor). Applicants undergo a “Classic Interview” with the EFRT Program Director, a student hired by the university to manage and oversee all team operations. The interview evaluates their passion for serving the community, and why they want to join the team. For the “Classic Interview” station, the rubric includes but is not limited to, sections on authenticity, communication skills, and general impressions. Last, there is one group station where the Executive Team, EFRT Responders hired by the Program Director, observes applicants’ teamwork, critical thinking, and problem-solving dynamics. For the group station, the rubric includes sections such as teamwork, skills/knowledge, communication, and general impression. After the MMIs, the Executive Team selects approximately 42 applicants to progress to Orientation (discussed in-depth in the ‘Selection’ section of the paper). See Figure 2 for a sample MMI schedule.
Figure 2: Sample MMI schedule
Phase 4: Orientation
Orientation includes nine days of intensive learning and practicing, giving applicants a glimpse into the nature and workload involved with volunteering on the EFRT. Orientation also allows the EFRT Responders to participate in the holistic evaluation of applicants.
Throughout Orientation, applicants are evaluated formally and informally (this is discussed in depth in the ‘Selection’ section of the paper). Responders are encouraged to comment on soft skills (e.g., professionalism, patient care, demeanor, work ethic, receptiveness to feedback) in addition to technical skills.
Phase 4A: Protocol Learning (Orientation 1)
Orientation begins with a two-day training, colloquially termed ‘Orientation 1,’ which standardizes applicants’ knowledge. Orientation 1 consists of lectures and small group activities teaching SFA, Basic Life Support (BLS), and elements of the EFRT’s protocol. The approximately 42 applicants are assigned into small groups of three applicants. Applicants work with their small group throughout Orientation and ultimately complete the group evaluation together. In small group sessions, the EFRT Responders with over one year of experience responding on the team clarify lecture content, discuss case studies, perform demonstrations, and deliver practice scenarios.
Orientation 1 equips applicants with the knowledge and skills needed for their formal evaluations. By incorporating the EFRT’s protocol during Orientation, we establish foundational skills for our future Junior Responders and test an applicant’s ability to learn and apply new information.
Phase 4B: Practice Sessions
Over the five days between Orientation 1 and the Formal Evaluations, Responders hold optional practice sessions for applicants, which allow applicants to apply their knowledge and improve their technical skills. Sessions include practice scenarios or skills practice. Responders provide constructive feedback and clarify any misunderstandings.
On the final practice session, applicants can attend one optional Executive
Member-led individual practice scenario. The standardized scenario represents the difficulty of the individual examination (Phase 4D) and concludes with the Executive Member providing the applicant with feedback.
Phase 4C and 4D Group Evaluation Group and Individual Evaluation (Orientation 2)
Final evaluations span two days: group evaluations on the first day and individual evaluations on the second. Applicants are expected to demonstrate their growth and learning throughout Orientation. Evaluations consist of simulated scenarios, similar to Observed Structured Clinical Examinations (OSCEs) seen in various healthcare training programs (Zayyan, 2011).
The scenarios used in the group and individual evaluations are created before Orientation. For the group evaluations, Responders are split into seven groups to create a scenario. The Training Coordinator, a member of the Executive Team, reviews all scenarios and ensures each scenario is standardized. For the individual evaluations, the Executive Team creates and standardizes the scenarios.
The small groups from Orientation 1 respond to seven simulated scenarios of varying topics taught throughout Orientation. Common topics include intoxication, physical trauma, mental health, and cardiac emergencies. Group evaluations assess applicants’ didactic, practical, communication, and teamwork skills in a high-stress environment. All EFRT Responders work together to evaluate scenarios. Similarly, individual evaluations have applicants respond to two simulated scenarios. Members of the Executive Team run the individual evaluations to provide insight into each applicant’s skills and knowledge.
Selection Process
Pre-Hiring Training
Before the EFRT’s application process begins, the Assistant Director and Training Coordinator create a presentation for ERFT Responders taking part in the hiring process. The Assistant Director is a Responder selected by the Program Director who sits on the Executive Team and is appointed to oversee many processes, one of which is Orientation. The presentation teaches Responders to create practice scenarios with intentions (e.g., practicing BLS skills) and explicit ‘Must-Sees’ and ‘Nice-to-Sees.’ ‘Must-Sees’ are actions that a Responder should meet within a set time limit to complete the scenario successfully. These are often actions that are pertinent to the patient’s survival. ‘Nice-to-Sees’ are actions that contribute to a positive patient interaction but do not change the patient’s survival outcome. For instance, in a heart attack scenario, a ‘Must-See’ would be assessing the need to administer aspirin, while a ‘Nice-to-See’ would be loosening tight clothing. The presentation includes a discussion of power dynamics and hiring biases to make EFRT Responders aware of the existing power dynamic between them and applicants.
Responders are encouraged to make decisions based on evidence and are taught about different types of biases to look out for (e.g., Confirmation Bias, Halo Effect, First Candidate Effect).
Responders are expected to be aware of any Conflict of Interests (COIs) they may have with applicants and are instructed to declare COIs to the Assistant Director. Responders do not evaluate COIs.
On-Going Evaluations
Evaluation occurs throughout Orientation and is conducted by all Responders. Non-Executive Responders act as a ‘pseudo-hiring panel.’ Non-Executive Responders work closely with applicants throughout the Orientation phases. Non-Executive Responders are encouraged to submit ‘Responder Testimonials’ throughout Orientation. ‘Responder Testimonials’ are a way to convey experiences with an applicant. Experiences can shed a positive or negative light on the applicant. Testimonials are objective and specific to the experience and include quotes, actions, and behaviors.
Group and Individual Evaluations
The group and individual evaluations are scored objectively. Responders who made the scenario standardize the rubric used for evaluations (i.e., it should be clear what criteria make a 1/5 different from a 2/5 score). During the scenarios, each applicant is evaluated on three criteria: skills/knowledge, communication/teamwork, and patient care. Each criterion is evaluated on a Likert Scale from 0 to 5 (e.g., 0 = unsatisfactory, 5 = EFRT Responder level).
For the individual evaluations, applicants are evaluated on a pass/fail basis. There are 4 evaluation outcomes: strong fail, weak fail, weak pass, or strong pass. An applicant reaches an outcome by comparing their performance to the scenarios’ ‘Must-Sees’ and ‘Nice-to-Sees.’ An applicant’s performance in their individual evaluation is compared to their scores from the group evaluations. This is used to understand the applicant holistically (i.e., to ensure they perform well individually in addition to in a team).
Once the scores from both days have been compiled, the Executive Team creates a list of the top-scoring 24 applicants. The Executive Team will refer to Responder Testimonials, interviews, and written applications when creating the list. This list is brought to a Team-Wide Selection Meeting.
Team-Wide Selection Meeting
At the Team-Wide Selection Meeting, a discussion is held on each applicant that made it to the ‘top 24.’ The Non-Executive Responders are unaware of applicant ranking and how the applicants performed in the individual scenarios to reduce biases. The Executive Team does not participate in this discussion. Responders only discuss specific experiences they had with an applicant (i.e., an applicant’s ability to implement feedback). The Executive Team listens
to the Responders’ discussion and asks follow-up questions as needed. A Non-Executive Responder is elected to ensure the discussion stays professional and objective. Responders with a COI for an applicant refrain from commenting until the end of the discussion.
Executive Team Selection Meeting
The Executive Team Selection Meeting looks at a combination of the final evaluation scores (indicative of technical skills) and comments from the Team-Wide Selection Meeting (indicative of soft skills). As seen in the EFRT’s 40 years of operations, Responders hired off of technical skills alone will respond well at the SFA level but may not flourish at the Emergency Medical Responder level (in which the EFRT operates). To ensure that the Executive Team hires applicants that will flourish, a high degree of skills must be demonstrated alongside growth, a willingness to learn, and teachability. Questions asked during this meeting include:
- Who will be able to provide optimal patient care?
- Who will be able to learn?
- Who will be committed to training?
- Who will take feedback well?
- Who fits the Emergency Medical Responder role while demonstrating strong resiliency?
This meeting culminates in picking 12-14 applicants to be hired onto the team. Two applicants are put on a waitlist in case of declined offers.
Inclusive & Equitable Hiring
In an umbrella review by Gomez and Bernet, patient outcomes improve with diverse healthcare teams (2019). The EFRT recognizes that being a group of diverse EMS responders helps us provide optimal care for the McMaster University campus. Introduced in 2023 to promote inclusive and equitable hiring, the EFRT has included a self-disclosure section on the written application for applicants to disclose their status within a marginalized community. Disclosures are not mandatory. Applicants can choose when and if they make a disclosure. Disclosures can be made at any time during the hiring process to any member of the Executive Team, and disclosures are kept confidential.
Self-disclosures do not put applicants at any disadvantage during the hiring process. Rather, self-disclosures may be used at points in the hiring process where decisions must be made regarding a tie between applicants. For example, when choosing applicants to progress to MMIs after the Written Test, if two applicants score the same, the Executive Team may choose to pick the applicants that reflect McMaster University’s commitment to building an intersectional inclusive community.
Admission & Retention
Admission into the EFRT is competitive, with an average acceptance rate of approximately 8.5% over the past four years. Approximately 90% of the total applicants who submit a written application are invited to the SFA Test, and from there, approximately 52-70% of applicants are invited to the MMIs. After the MMIs, approximately 50% of applicants move on to Orientation. The hiring process concludes with 12-14 applicants selected each cycle. See Table 1 for a breakdown of applicants at each stage, including data spanning the past four years (2020-2023).
Table 1: Admission & Retention
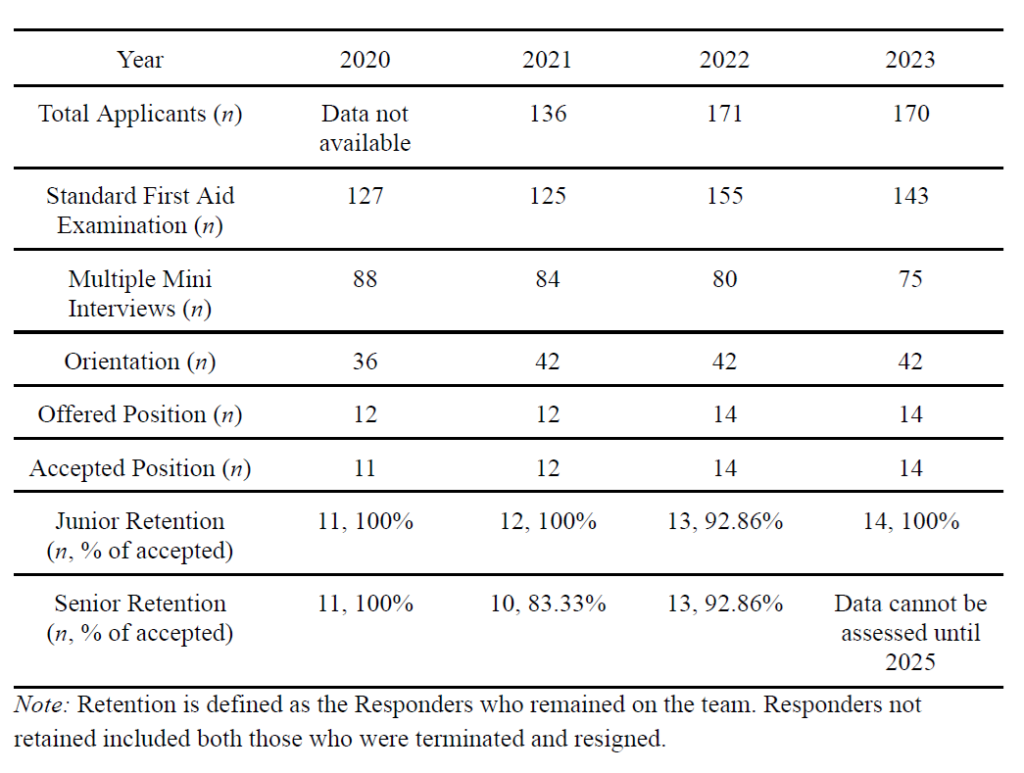
The EFRT has retention rates ranging from 93-100% in junior cohorts (within the first year of responding) and 83-100% in senior cohorts (the remainder of their
time on the team prior to graduation). In our opinion, we attribute our team’s high retention to the success of the Orientation process, which is two-fold in its realistic portrayal of our responsibilities and commitment as Responders, and its accuracy in identifying individuals with substantial potential as Responders, encompassing both their soft skills and first-aid proficiency. First, despite the time investment demanded from both applicants and current Responders, we believe that the high degree of dedication and time commitment required from applicants accurately portrays what is required of a collegiate EMS responder. As such, the successful applicants are those who demonstrate dedication and time to practicing and improving their skills. Furthermore, given the comprehensive nature of our five-stage evaluation process, our team believes we possess ample insight into the applicants to comprehend their potential as a Responder. See Table 1 for a breakdown of retention rates, including data spanning the past four years (2020-2024).
Conclusion
McMaster University’s EFRT has established a comprehensive and highly selective hiring process to ensure Junior Responders are resilient and well-prepared to handle the demanding nature of collegiate EMS. Using a multi-phase selection method, we identify applicants with the necessary technical and soft skills. We strongly believe that this method enhances the quality of care provided to our community and contributes to the
EFRT’s exemplary retention rates. Other collegiate EMS teams facing retention challenges may find it useful to adopt or adapt our hiring process to build a team of resilient EMS responders that can withstand the demands of their role.
Acknowledgements
The authors would like to thank the EFRT and the many talented responders who have dedicated their time and expertise to developing this hiring process.
References
Gomez, L. E., & Bernet, P. (2019). Diversity improves performance and outcomes. Journal of the National Medical Association, 111(4), 383–392. https://doi.org/10.1016/j.jnma.2019.01.006
Hall, L. H., Johnson, J., Watt, I., Tsipa, A., & O’Connor, D. B. (2016). Healthcare staff wellbeing, burnout, and patient safety: A systematic review. PloS ONE, 11(7), e0159015. https://doi.org/10.1371/journal.pone.0159015
The Canadian Red Cross Society. (2024). Knowledge evaluation. Canadian Red Cross. https://lms.redcross.ca/boulevard/evaluation
Zayyan, M. (2011). Objective structured clinical examination: The assessment of choice. Oman Medical Journal, 26(4), 219-222. https://doi.org/10.5001/omj.2011.55
Author & Article Information
Marion Miguel Antazo, BHSc, EMR is a graduate of McMaster University’s Honours Biochemistry program, and is currently a Physician Assistant candidate at the University of Toronto. Marion has served on McMaster’s Emergency First Response Team for three years. Marina N. Fonseca, EMR graduated from McMaster University’s Health Sciences program (BHSc), and is a candidate for McMaster University’s Applied Psychology program (BASc). Marina has served on McMaster’s Emergency First Response Team for four years. Fezan Khokhar, BSc, EMR is a graduate of McMaster University and was on the Emergency First Response Team (EFRT) for 4 years and was the 2023-2024 Program Director. Fezan currently sits on the EFRT advisory board and is a MD Candidate at the University of Toronto. Mellina J. Solomon, EMR is the 2024-2025 Assistant Director at McMaster University’s Emergency First Response Team and a fourth-year student at McMaster University graduating with a B.Sc in Psychology, Neuroscience and Behaviour. Mellina is in her fourth year with McMaster’s Emergency First Response Team.
Author Affiliations: From McMaster University Emergency First Response Team – in Hamilton, Ontario, Canada (M.M.A., M.N.F., F.K., M.J.S.).
Address for Correspondence: Mellina J. Solomon | Email: mellinasolomon@gmail.com
Conflicts of Interest/Funding Sources: By the JCEMS Submission Declaration Form, all authors are required to disclose all potential conflicts of interest and funding sources. All authors declared no conflicts of interest. All authors declared that they did not receive funding to conduct this research and/or associated with this work.
Authorship Criteria: By the JCEMS Submission Declaration Form, all authors are required to attest to meeting the four ICMJE.org authorship criteria: (1) Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND (2) Drafting the work or revising it critically for important intellectual content; AND (3) Final approval of the version to be published; AND (4) Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Submission History: Received June 20, 2024; accepted for publication July 29, 2024
Published Online: September 9, 2024
Published in Print: Pending
Reviewer Information: In accordance with JCEMS editorial policy, Advice and Practice manuscripts are reviewed by the JCEMS Editorial Board and, as needed, independent reviewers. JCEMS thanks the Editorial Board members and independent reviewers who contributed to the review of this work.
Copyright: © 2024 Antazo, Fonseca, Khokhar, & Solomon. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International (CC BY 4.0) License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. The full license is available at: https://creativecommons.org/licenses/by/4.0/
Electronic Link: Pending