Abstract
Background: Collegiate-based emergency medical services (CBEMS) agencies are a unique service model within the world of emergency medical services (EMS). CBEMS agencies vary widely concerning organizational, operational, and other characteristics. The financial setups of these groups are also varied, but not well documented. Objectives: The purpose of this study was to examine determinants of budget size and budget sources for a cross-section of CBEMS agencies. Methods: An electronic survey was sent to volunteer CBEMS agencies using the National Collegiate Emergency Medical Services Foundation (NCEMSF) database. The survey requested agency demographics and budget data. Results were collected and analyzed using a chi-square test. Results: Large student body populations, agencies that transport patients, 24/7 response agencies, and agencies with high annual call volumes were associated with larger budgets. Most CBEMS agencies received the bulk of their funds from their institution and few relied on fundraising. Conclusion: Many disparate factors affect CBEMS’s budget size. CBEMS agencies exhibit high levels of diversity in budget size, operational characteristics, and fundraising strategies. Access to peer agency information will allow CBEMS agencies to build and maintain well-funded organizations.
Introduction
Collegiate-based emergency medical services (CBEMS) agencies play an important role in keeping campus communities healthy and safe by providing quality emergency medical treatment. Like the colleges and universities they serve, CBEMS agencies are unique. Their idiosyncrasies have been captured in past surveys as well as by the EMS Organization Database hosted on the National Collegiate Emergency Medical Services Foundation (NCEMSF) website.1-6 Some agencies transport their patients via ambulance, while others escalate care to on-site advanced life support (ALS) services or call 911. Some are staffed by emergency medical technicians (EMTs), while a minority employ paramedics.5 Annual call volume can range from less than 100 to over 1,000.5
CBEMS agencies also differ with respect to budget size and source.4, 5, 7 Literature has shown that CBEMS agency budget size has a large range.5, 7 Funding variations could have real-world consequences, specifically if agency operations are constrained by a lack of funds. Funding problems can damage emergency medical services (EMS) systems in general, and CBEMS systems in particular.8 For example, budget cuts are correlated with an increased mean response time for CBEMS agencies.7 Budget sources for CBEMS agencies have been investigated, but the percentage contribution to the total budget of individual sources has not.4
This effort builds on previous demographic surveys to describe the financial details of surveyed CBEMS agencies in more depth. The goals of this project are to begin a detailed discussion on CBEMS funding and to serve as a reference for new or existing CBEMS agencies looking to contextualize their finances.
Methods
Figure 1: CBEMS agencies were identified and screened before survey release, and again post-survey. Reasons for exclusion are enumerated at each screening step. This process was based on the PRISMA method.16
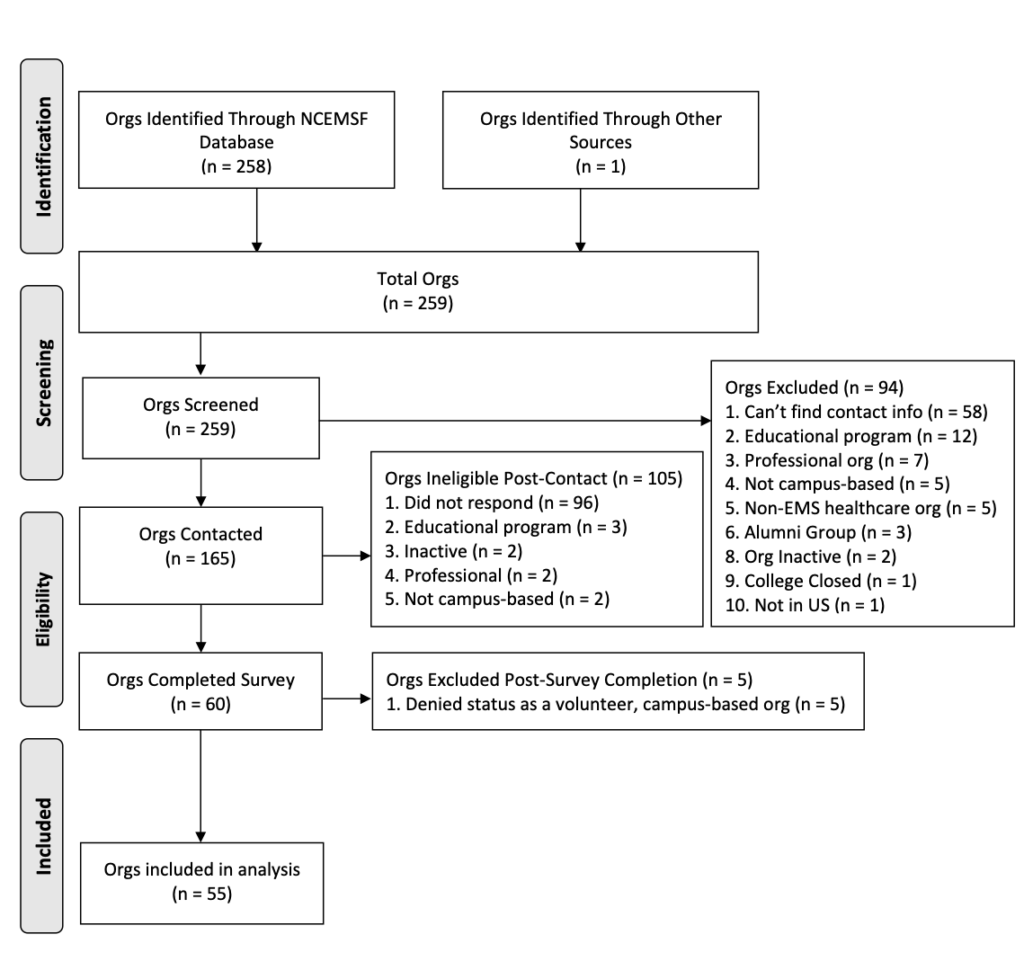
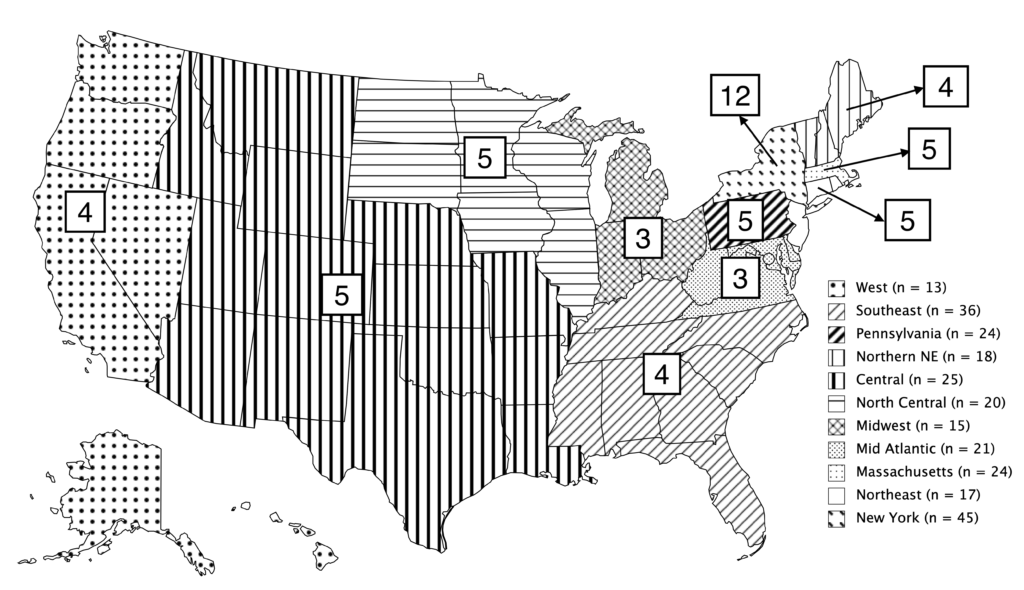
The survey was developed using Google Forms and distributed electronically to CBEMS agencies listed on the NCEMSF United States EMS Organizations webpage through 11 NCEMSF Regional Coordinators.6 Through this method, 1 additional CBEMS agency not listed on the NCEMSF webpage responded to the survey. In parallel, 165 target agencies were contacted at least twice over 4 months (Figure 1). After contact, 105 organizations were rendered ineligible, most (96 agencies, 58%) because they failed to complete the survey. 60 organizations completed the survey, for a response rate of 36%, with 5 organizations excluded from analysis. 55 agencies made up the study (Figure 2).
Figure 2: Regional locations of the 55 CBEMS agencies in the study. Boxed numbers are the number of agencies in that region recruited to the study. Legend indicates the total agencies per region in the NCEMSF US database. Figure created using mapchart.net.
Historically, it has been difficult to survey the CBEMS community due to personnel turnover. Emphasis was placed on making the survey brief to increase response rates.9 Professional EMS agencies were screened out by survey respondents affirming they belonged to an all-volunteer agency. The full survey transcript can be found in Supplementary Materials. Survey respondent privacy is protected by only publishing anonymized statistics. IRB review of this project was deemed not necessary by the Research Compliance Office at Stanford University.
Graphical representations were created using Microsoft Excel. Chi-square analyses were performed using R. Frequency rates are often shown as percentages of the total amount in that category, to account for different amounts of respondents in each category. Statistical significance was set at p<0.05.
Results
Table 1: Survey respondent demographics are shown as values and percentages. CBEMS agencies that skipped answering a question or the question didn’t apply to their organization were not counted. Respondents with multiple answers to a question were counted for each answer.
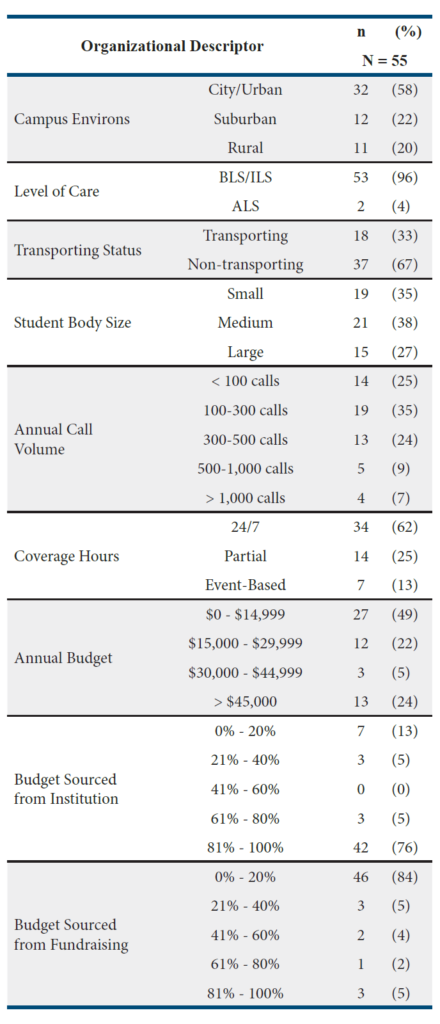
CBEMS Agency Characteristics
Demographics of survey respondents are seen in Table 1. The vast majority operated at basic life support (BLS) or intermediate life support (ILS) levels, with 4% providing ALS. Two-thirds were non-transporting services, while one-third provided medical transport. CBEMS agencies were divided into three bins based on their campus student population.10 Annual call volume was measured. Agencies were allowed to select multiple types of coverage hours.
Figure 3: Student Body and Budget Size. Size of the tertiary educational institution related to budget size of the CBEMS agency that serves its campus. Colleges and universities were split into 3 size categories based on the total student population.10 Groups were plotted as frequency percentages within that size category (see Methods).
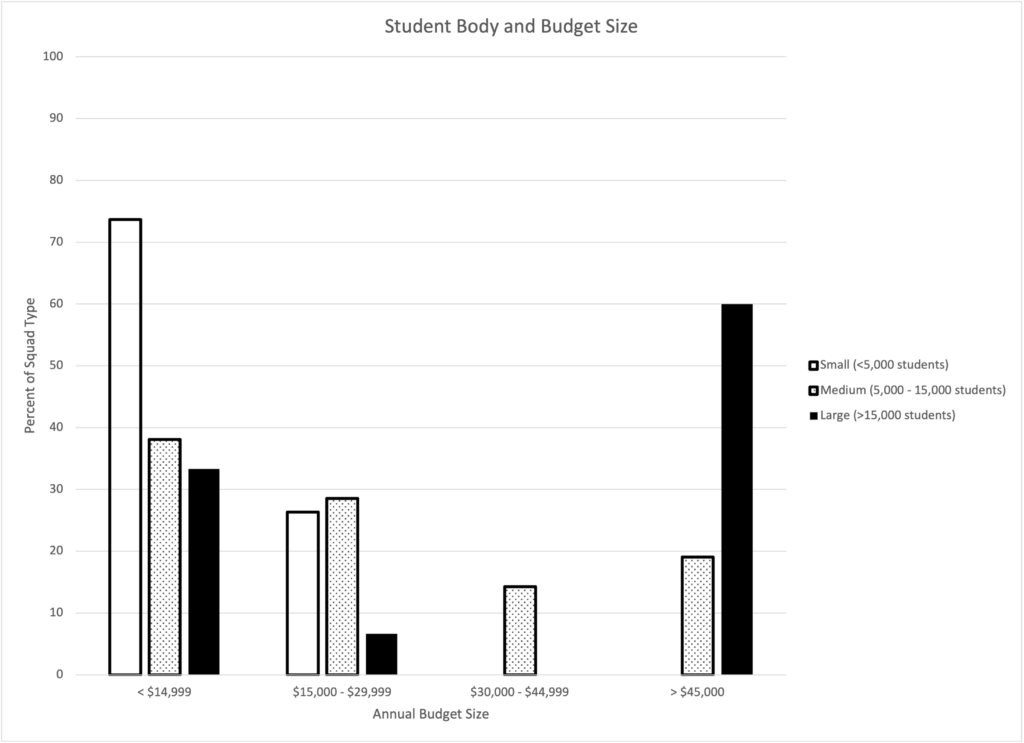
Campus Student Body and Budget Size
Student body size was significantly related to budget size, X2(6, N = 55) = 23.7, p < .001 (Figure 3). Generally, large campus CBEMS agencies had the largest budgets, followed by medium campuses, then small. Large campus groups had a bimodal budget distribution, with the majority of groups (60%) over $45,000 annually, and 33% accessing less than $15,000. Medium CBEMS agencies had a more balanced distribution. The most common budget bin for agencies at medium-sized schools was $0 – $14,999, with 38% of agencies at this size. Besides that bin, none other captured more than 30% of medium-size school CBEMS agencies. CBEMS agencies at small schools generally had the smallest budgets, none accessing more than $30,000 annually, and 74% having budgets smaller than $15,000.
Figure 4: Transportation Status and Budget Size. Budget size of transporting and non-transporting agencies. Transporting agencies were defined as those who can take their patients directly to the hospital. Data are plotted as frequency percentages within each category (see Methods).
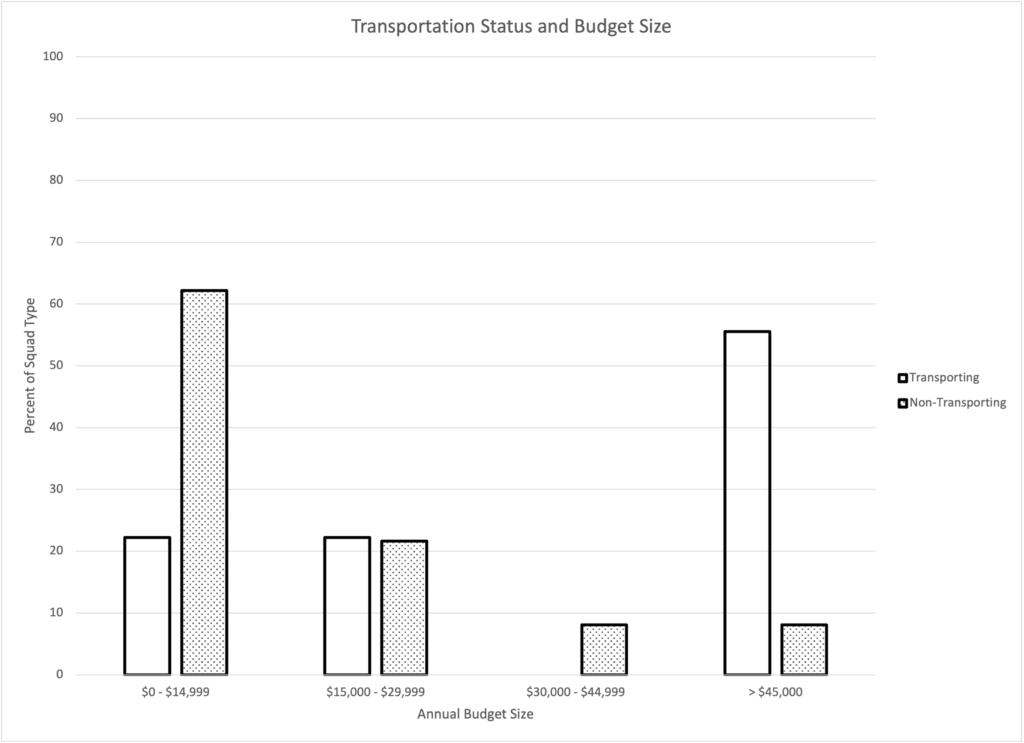
Transporting versus Non-Transporting Agencies
Transportation status was significantly related to budget size, X2(3, N = 55) = 16.9, p < .001 (Figure 4). Transporting agencies generally had larger budgets than non-transporting agencies. Most (56%) transporting agencies had budgets greater than $45,000. Only 8% of non-transporting agencies had budgets of this size. Most (62%) non-transporting agencies had budgets less than $15,000. Middling budget sizes, between $15,000 – $45,000, saw closer rates of transporting (22%) and non-transporting (30%) agencies.
Figure 5: Call Volume and Budget Size. Call volume of the CBEMS agency related to its budget size. CBEMS agencies were split into 5 populations based on call volumes. Data are plotted as frequency percentages within each call volume category (see Methods).
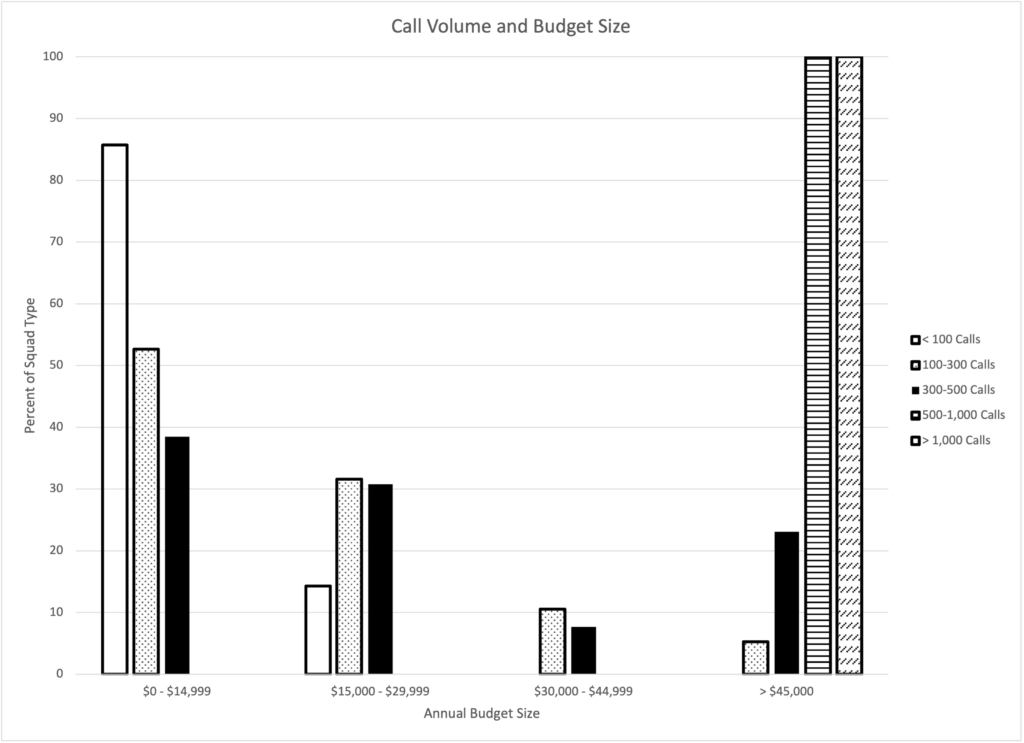
Call Volume and Budget Size
Call volume was significantly related to budget size, X2(12, N = 55) = 42.7, p < .001 (Figure 5). Budget size generally increased with call volume for CBEMS agencies. All agencies in the two highest call volume brackets also had budgets over $45,000. Agencies with 300-500 calls were more evenly distributed, with no one budget category having more than 40% of those agencies. 100-300 call agencies all had budgets under $40,000, except for one outlier with a budget over $100,000. Agencies with less than 100 calls all had budgets under $20,000.
Figure 6: Coverage Hours and Budget Size. Budget sizes of CBEMS agencies with different coverage hours are shown. The coverage hours represent aggregated survey bin options: 24/7 (24/7 calendar year, 24/7 academic year); partial hours (nightly, nightly calendar year, nightly academic year, limited daily hours academic year, limited daily hours calendar year, weekends academic year, weekends calendar year); events (event-based). Groups were plotted as frequency percentages within each coverage category (see Methods).
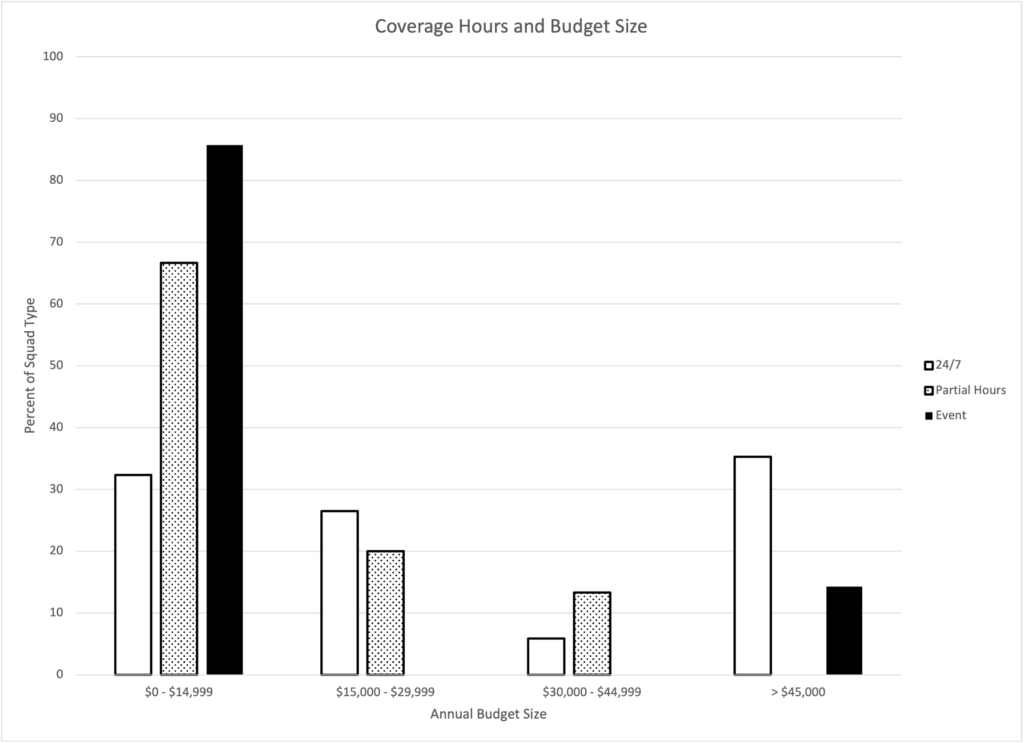
Coverage Hours and Budget Size
Coverage hour schedules are significantly related to budget size, X2(6, N = 55) = 14.0, p = .03 (Figure 6). Generally, the more coverage hours a CBEMS agency offers, the larger its budget. Only 32% of 24/7 agencies have budgets under $15,000, compared to 67% of partial hours squads and 86% of event-based groups. In the middling budget range, between $15,000 and $45,000, there was an almost equal distribution between 24/7 (32%) and partial hours (33%) groups. At the high end, with budgets greater than $45,000, the largest group of 24/7 squads existed (35%).
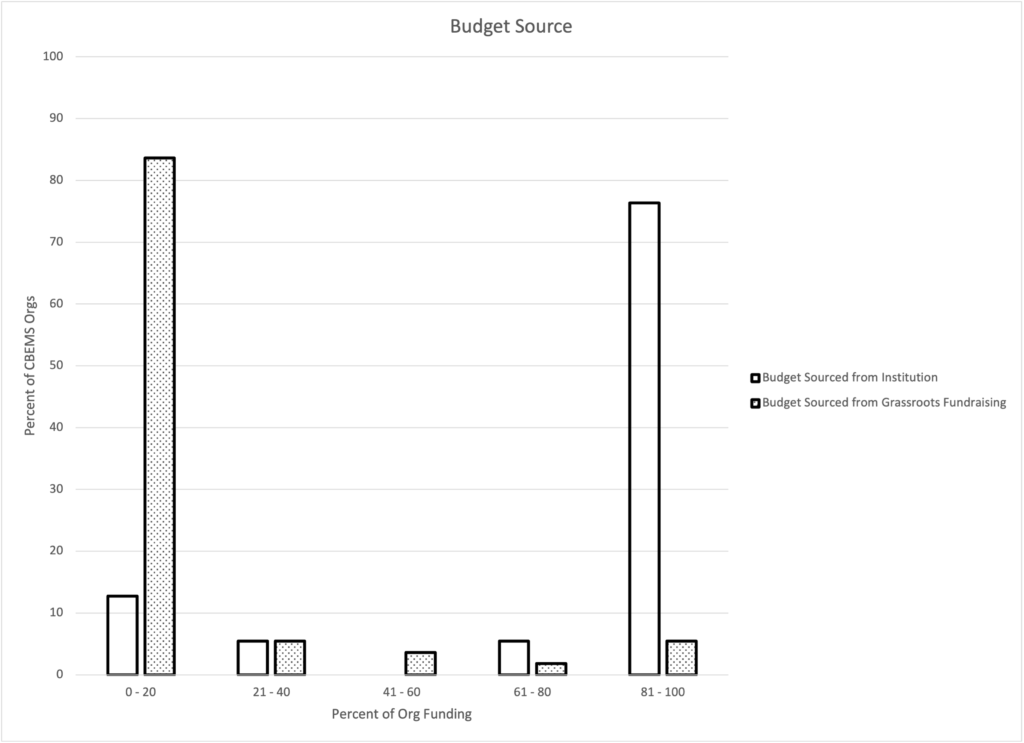
Figure 7: Budget Source. The percentage of CBEMS budgets coming from the institution itself and grassroots fundraising. Institutional funding includes all funds supplied by the college or university itself, while grassroots fundraising includes funds gathered from teaching CPR classes, soliciting donations, or other acts undertaken by the CBEMS agency to collect money.
Source of Budget Funds
CBEMS agencies received most, if not all, of their funding from their higher education institution, and fundraised very little for their annual budget (Figure 7). Most (76%) CBEMS agencies got 81%-100% of their budget from their institution, and 84% had to fundraise only 0%-20% of their annual budget.
Discussion
Like the field of EMS as a whole, the origins of collegiate EMS are relatively recent. CBEMS agencies first formed in the emergency medical boom of the late 20th century, with limited information available on early groups.1,11-13 Initially without a national guiding organization, almost no literature existed discussing the details of CBEMS operation.14 Present-day diversity in CBEMS financials could be linked to limited research during the field’s inception. Illustrative of this is the CBEMS mean annual budget of $39,333.38 (STD = $106,217.20, n=101).5 The large standard deviation suggests variety in budget size. Our data show a relationship between CBEMS budget size and student population, with the most populated campuses having the highest funded CBEMS agencies. Serving a larger student body could involve higher call volume, larger squad size and campus area, and corresponding equipment and vehicle costs.
Similar explanations could be behind our other findings. Our results suggest that transporting agencies generally have higher budgets than non-transporting agencies. Owning, maintaining, staffing, and fueling a transport vehicle can come at a high cost, a potential cause for this relationship.15 Our data show that budget size generally increased with call volume. Responding to calls requires manpower, equipment, and being in service, all of which can impact the bottom line. 24-hour service tends to be the most expensive coverage scheme, with 24/7 squads in service for longer than their partial hours or event-based colleagues. Longer hours require more staffing and could be tied to an increase in patients seen due to a larger temporal catchment.
Funding from the university generally provided most or all monies for many CBEMS budgets, consistent with prior findings.4 Within higher education, there are many ways to secure funding. Some organizations are paid via the general fund (tuition), health fees, student fees, or operating budgets of the campus health office or department of public safety.14
The aforementioned trends appear to link together consistently. Larger budgets are linked with agencies who provide more medical care, whether that is through more service hours, a higher call volume, or offering transport, among other factors. While these data cannot discern causality, and said factors seem to be closely interconnected, it seems that the size of an agency’s budget is to a certain degree a function of the scope of the agency’s role in the community. One presumed causal relationship could be agencies who expand the scope of their operations are rewarded with attention and funding from their institution. Conversely, additional funding could pre-empt and support the expansion of CBEMS operations. Therefore, CBEMS agencies looking to establish or grow their service have options in discussions with administration. They could offer additional services to justify increased budgets in the future. They could also show the administration what additional funds would allow them to accomplish. We encourage CBEMS agencies and college administrators to use these data when discussing the desired role and scope of an agency, and the commensurate budget needs.
These results suggest the need for further research and comparison across the financial landscape of collegiate EMS. In higher education and healthcare, comparison between peer institutions is used to create standards, ensure competition and innovation, and drive the field forward. Research that looks into fundraising models (donations, CPR classes, etc.), gets granular non-binned data, or considers other variables (organization membership size, fee for service, etc.) is welcomed. Low survey completion rates due to incorrect contact information suggest that an update of the NCEMSF US Organization Database would prove useful. Allowing organizations to easily contact each other, build bonds, share information, and conduct research, would grow the NCEMSF on a national scale, and improve local CBEMS agencies. Healthy finances are important for CBEMS agencies, as underfunding can impact the ability of CBEMS agencies to provide quality emergency medical care.7 Hopefully, these results will serve as a useful guide for existing or emergent CBEMS agencies, leadership teams, school administrators, and other stakeholders to refer to when discussing finances.
Limitations
This work adds to a limited base of CBEMS budget research. While not definitive, our study encourages further investigation in the field. Results cannot be extrapolated to professional agencies or groups outside the US. The scope of this study did not include analysis of the full financial complexity of a CBEMS budget. Volunteer agencies often receive valuable non-monetary contributions from their institution or outside sources that were not measured in this survey.1,11 These contributions could include free or discounted operational real estate on campus grounds, training, uniforms, and food.
Sample size and respondent bias also limit this work (Figure 1). It is likely the 55 respondents are not perfectly representative of all-volunteer CBEMS agencies. Well-funded and established CBEMS agencies with dedicated websites, social media accounts, and permanent email addresses, may have been more likely to be reached by the survey. Agencies in flux or out of service due to the COVID-19 pandemic were less likely to answer the survey. Difficulty in contacting NCEMSF agencies calls for comprehensive efforts to gather updated demographic and contact information.
Binning of survey data limits the statistical interpretations that can be performed. Data could be skewed within a bin. Binning was a calculated decision in survey design that encouraged survey completion by making the survey faster to complete.9 While the trends are well illustrated by the histograms seen in this paper, further studies using continuous values could elucidate more specific information about CBEMS budgets.
This work adds to a limited base of CBEMS budget research. While not definitive, our study encourages further investigation in the field. Results cannot be extrapolated to professional agencies or groups outside the US. The scope of this study did not include analysis of the full financial complexity of a CBEMS budget. Volunteer agencies often receive valuable non-monetary contributions from their institution or outside sources that were not measured in this survey.1,11 These contributions could include free or discounted operational real estate on campus grounds, training, uniforms, and food.
Sample size and respondent bias also limit this work (Figure 1). It is likely the 55 respondents are not perfectly representative of all-volunteer CBEMS agencies. Well-funded and established CBEMS agencies with dedicated websites, social media accounts, and permanent email addresses, may have been more likely to be reached by the survey. Agencies in flux or out of service due to the COVID-19 pandemic were less likely to answer the survey. Difficulty in contacting NCEMSF agencies calls for comprehensive efforts to gather updated demographic and contact information.
Binning of survey data limits the statistical interpretations that can be performed. Data could be skewed within a bin. Binning was a calculated decision in survey design that encouraged survey completion by making the survey faster to complete.9 While the trends are well illustrated by the histograms seen in this paper, further studies using continuous values could elucidate more specific information about CBEMS budgets.
Conclusion
CBEMS agencies have budgets that are as unique and diverse as the organizations themselves. A demographically widespread group of CBEMS agencies were surveyed about their budget size and sources of funding. Larger student populations, longer coverage hours, transporting agencies, and higher call volumes were more often served by CBEMS agencies with larger budgets. Inversely, smaller student populations, limited coverage times, non-transporting agencies, and low call volumes were associated with lower budgets. CBEMS agencies commonly receive most or all of their budget funds from their host institution, and rarely fundraise a large part of their budget. Small sample sizes, survey respondent bias, and non-financial budgetary elements limit the interpretability of this study. The importance of adequate funding for CBEMS agencies necessitates that agencies have better access to peer agency information to build and maintain quality organizations that continue to deliver high-value care to campus communities.
Acknowledgments
The authors would like to thank all survey participants for their diligence in providing accurate information, Michael Beautyman for his assistance in compiling the research team, and Patrick Atkinson for advice on statistical methods. The authors declare no financial support for the research, authorship, or publication of this article. The authors declare no conflicts of interest.
References
- Wang J. Investigating the Current Status of Collegiate Emergency Medical Services (EMS) Organizations via a National Survey Study. ASU Electronic Theses and Dissertations. 2019.
- King BR, Zachariah BS, Cone DC, Clark P. A survey of emergency medical services systems on college and university campuses. Prehospital Disaster Medicine. 1996;11(4):265-269. doi:10.1017/s1049023x00043107
- Fisher J, Ray A, Milliron ME, Koenig GJ. Campus Based EMS: A Survey by the National Collegiate EMS Foundation. Oral Presentations of the Mediterranean Emergency Medicine Congress. 2003:6.
- Fisher J, Ray A, Savett SC, Milliron ME, Koenig GJ. Collegiate-based emergency medical services (EMS): A survey of EMS systems on college campuses. Prehospital Disaster Medicine. 2006;21(2):91-96. doi:10.1017/s1049023x00003411
- Wolbrom DH, Rahman AM, Hilton MT. A Survey of 200 National Collegiate Emergency Medical Service Organizations. Prehospital Disaster Medicine. 2017;32(S1):S170-S171. doi:10.1017/S1049023X17004575
- EMS Organization Database. National Collegiate Emergency Medical Services. Accessed January 15, 2021.
- D.H. W, Rahman AM, M.T. H. Underfunding of collegiate emergency medical services strains the delivery of adequate prehospital care. Academic Emergency Medicine. 2017;24:S230-S231. doi:10.1111/acem.13203
- Heightman AJ. Understanding Why EMS Systems Fail. Journal of Emergency Medical Services. 2015;40(2).
- Kost RG, Correa da Rosa J. Impact of survey length and compensation on validity, reliability, and sample characteristics for Ultrashort-, Short-, and Long-Research Participant Perception Surveys. Journal of Clinical and Translational Science. 2018;2(1):31-37. doi:10.1017/cts.2018.18.
- College Sizes: Small, Medium, or Large. College Data. Accessed January 21, 2021.
- Struve OAM. Design and Implementation of a Sustainable, University-Based, Emergency Medical Response Service. USF Theses Digital Repository. 2014.
- Accidental Death and Disability: The Neglected Disease of Modern Society. National Academy of Sciences and National Research Council. 1966. doi:10.17226/9978.
- Mission and History. National Collegiate Emergency Medical Services Foundation. Accessed January 15, 2021.
- Delorenzo RA, Gray BC. Emergency medicine on college campuses: Key elements in the establishment and -success of a campus-based ambulance corps. Journal of American College Health Association. 1986;35(2):92-93. doi:10.1080/07448481.1986.9938968
- Lindberg, A., 2011. How Much Does an Ambulance Cost?. Tampa Bay Times. Accessed 26 February 2021.
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Medicine. 2009;6(7). doi:10.1371/journal.pmed.1000097
Author & Article Information
Murray J. Bartho, BS, EMT, is a hearing loss researcher at Stanford University and volunteer EMT with Stanford EMS. He has served as Director of Logistics for Stanford EMS and as Operations Officer for Santa Clara University EMS. Tom Goode, MS, EMT, works as a statistical analyst at the RAND Corporation and as an EMT with the Munhall Area Prehospital Services. Gabe Gan, MPH, NRP, works as a management and program analyst at the DC Fire and EMS Department. He is a volunteer Paramedic with the Silver Spring Volunteer Fire Department.
Author Affiliations: From Stanford University School of Medicine – in Stanford, CA (M.J.B.). From RAND Corporation; Munhall Area Prehospital Services – in Homestead, PA (T.G.). From DC Fire and EMS Department; Silver Spring Volunteer Fire Department – in Washington, D.C.; Silver Spring, MD (G.G.).
Address for Correspondence: Murray J. Bartho, BS, EMT | Email: mbartho@stanford.edu | Phone: +1 (503) 729-2011 | Mailing Address: 3620 Olson Court, Lake Oswego, OR 97034
Conflicts of Interest/Funding Sources: By the JCEMS Submission Declaration Form, all authors are required to disclose all potential conflicts of interest and funding sources. All authors declared that they have no conflicts of interest. All authors declared that they did not receive funding to conduct the research and/or writing associated with this work.
Authorship Criteria: By the JCEMS Submission Declaration Form, all authors are required to attest to meeting the four ICMJE.org authorship criteria: (1) Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND (2) Drafting the work or revising it critically for important intellectual content; AND (3) Final approval of the version to be published; AND (4) Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Submission History: Received March 2, 2021; accepted for publication September 3, 2021.
Published Online: October 31, 2021
Published in Print: October 31, 2021 (Volume 4: Issue 2)
Reviewer Information: In accordance with JCEMS editorial policy, Original Research manuscripts undergo double-blind peer-review by at least two independent reviewers. JCEMS thanks the anonymous reviewers who contributed to the review of this work.
Copyright: © 2021 Bartho, Goode & Gan. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International (CC BY 4.0) License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. The full license is available at: https://creativecommons.org/licenses/by/4.0/
Electronic Link: https://doi.org/10.30542/JCEMS.2021.04.02.04